Factors determining change of antibiotic and prolong hospital stay in children with severe pneumonia in a tertiary care hospital, Dhaka, Bangladesh
Abstract
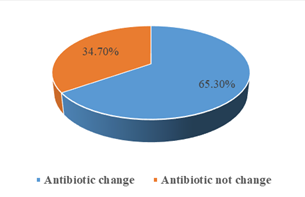
Background: Pneumonia is one of the most common infections in the pediatric age group and one of the leading diagnoses that results in hospital admission for children. Severe pneumonia remains a common and serious condition worldwide. Various micro-organisms can cause pneumonia, and etiologies differ by age. Clinical manifestations vary, and diagnostic testing is frequently not standardized. Objective: To identify the factors determining the need of antibiotic change and prolong hospital stay in children Under Five Years of Age Hospitalized with Severe Pneumonia. Study design: Prospective observational cohort study. Study place and period: Dhaka Shishu (Children) Hospital, Dhaka, from December 2012 to May 2013. Study population: Children under 5 years of age admitted with severe pneumonia. Sample size: n= One Hundred Fifty included. Methods/ Procedure: All the data was collected and recorded systematically in a questionnaire and was analyzed using computer software SPSS (Statistical package for social sciences) and analysis was multivariate to find out the significant factors. Main outcome measures: Change of antibiotic and prolong hospital stay, in children Under Five Years of Age Hospitalized with Severe Pneumonia of this study. Results: The mean age was found 9.49±6.83 months with range from 2 months to 36 months and Male to female ratio was 2:1. The duration of hospital stay was >5 days in almost two third (62.7%) of the patients. The mean age of the mothers was 24.67±4.19 years. Regarding study of association of different factors with prolong hospital stay it was observed that patients who needed prolong hospital stay 53.2% of them live in an overcrowded environment and 32.1% patients live in an overcrowded environment who didn`t need prolong hospital stay. Among 150 study patients, 98(65.3%) needed a change in antibiotics, 94(62.7%) patients needed more than 5 days’ hospital stay. 34.7% of patients were exclusively breast fed of those who needed a change in antibiotic and 80.8% among those who didn`t need any change. 85.7% presented with head nodding among those who needed antibiotic change, on the other hand, 19.2% with head-nodding among those who didn`t need antibiotic change. Leukocytosis was found in 57.1% and 19.2% among patients who needed a change of antibiotics and didn`t need antibiotic change respectively. In patients who needed a change of antibiotic, positive blood culture was found in 20.4% of cases and it was 0% among patients who didn`t need a change. Radiological abnormality was found in 87.8% of patients who needed antibiotic change and 42.3% in patients who didn`t need antibiotic change. Statistically significant (p<0.05) factors associated with two groups of patients those who needed a change of antibiotics and those who didn`t need are overcrowding, exclusive breastfeeding, head nodding on presentation, leukocytosis, positive blood culture, and abnormal CXR. Conclusion: Children hospitalized with severe community-acquired pneumonia [as defined by World Health Organization (WHO)] who had not received exclusive breastfeeding, had stayed in overcrowded homes and had an abnormal chest radiograph were more likely to fail to respond with the primary antibiotic regimen and require change of antibiotics and prolonged hospital stay.
Downloads
References
Charles C. Prober, Theodore C. Sectish. Pneumonia. In: Behrman RE, Kliegman RM, Jenson HB, Stanton BF (editors). Nelson Textbook of Paediatrics (18th Edition). Philadelphia: WB Saunders Company, 2007. pp. 1795-9.
Hospital care for children. World health organization, 2005. Available: http://whqlibdoc.who.int/publications/ 2005/9241546700.pdf. Accessed: 19 November 2012.
Pneumonia: The forgotten killer of children: WHO/UNICEF, 2006. Available: www.unicef.org/publications/index_ 35626. HTML. Accessed: 19 November 2012.
Tiewsoh K, Lodha R, Pandey RM, Broor S, Kalaivani M, Sushil K Kabra. Factors determining the outcome of children hospitalized with severe pneumonia. BMC pediatrics 2009; 9:15.
Bangladesh Demographic Health Survey 2004, Ministry of Health, Bangladesh. Available: www. measuredhs.com/pubs/ pdf/FR165/FR-BD04[FR165].pdf. Accessed: 19 November 2012.
Moine P, Vercken JB, Chevret S, Chastang C, Gajdos P. Severe community-acquired pneumonia etiology, epidemiology and prognosis factors. Chest 1994; 105: 1487-95.
Sehgal V, Sethi GR, Sachdev HP, Satyanarayana L. Predictors of mortality in subjects hospitalized with lower respiratory tract infections. Indian Pediatrics 1997; 34: 213-9.
Feldman C, Viljoen E, Morar R, Richards G, Sawyer L, Goolam Mahomed A. Prognostic factors in severe community-acquired pneumonia in patients without co-morbid illness. Respirology 2001; 6: 323-30.
Roth DE, Caulfield LE, Ezzati M, Black RE. Acute lower respiratory infections in childhood: opportunities for reducing the global burden through nutritional interventions. Bulletin of the World Health Organization 2008; 86: 356-364.
Madhi SA, Levine OS, Hajjeh R, Mansoor OD, Cherian T. Vaccines to prevent pneumonia and improve child survival. Bulletin of the World Health Organization 2008; 86: 365-372.
Rudan I, Boschi-Pinto C, Biloglav Z, Mulhollandd K, Campbelle H. Epidemiology and etiology of childhood pneumonia. Bulletin of the World Health Organization 2008; 86: 408-416.
Lee JH, Ryu YJ, Chun EM, Chang JH. Outcomes and Prognostic Factors for Severe Community-Acquired Pneumonia that Requires Mechanical Ventilation. The Korean Journal of Internal Medicine 2007; 22: 157-163.
Park K. Park's Textbook of Preventive and Social Medicine Sixteenth edition. jabalpur, Banarasidas Bhanot and company; 2006:521.
Uddin KMF, Jahan N, Mannan MA, Ferdousi SA, Farhana T, Akhter S, Alam R. Risk Factors Determining the Outcome of 2-12 Months Age Group Infants Hospitalized with Severe Pneumonia. Medicine 2013; 25(01), pp. 9-13.
Ramachandran P, Nedunchelian K, Vengatesan and Suresh S. Risk Factors for Mortality in Community –Acquired Pneumonia Among Children Aged 1-59 Months Admitted in a Referral Hospital. Indian Pediatrics 2012; 49: 889-895.
Andersson R, Olomi R. Pneumonia among hospitalized children aged 1-9 years. Peter Forsberg, medical student at the Sahlgrenska Academy at Gothenburg University, Sweden 2012; 1-27.
Shah N, Ramankutty V, Premila PG, Sathy N: Risk factors for severe pneumonia in children in south Kerala: a hospitalbased case-control study. J Trop Pediatr 1994; 40: 201-206.
Coles CL, Fraser D, Givon-Lavi N, Greenberg D, Gorodischer R, Bar-Ziv J, Dagan R: Nutritional status and diarrheal illness as independent risk factors for alveolar pneumonia. Am J Epidemiol 2005; 162: 999-1007.
Suwanjutha S, Ruangkanchanasetr S, Chantarojanasini T, Ttotrakitya S. Risk factors associated with morbidity and mortality of pneumonia in children under 5 years. Southeast Asian J Trop Med Public Health 1994; 25(1): 60-66.
Gálvez CA, Modeste N, Lee JW, Betancourt H, Wilkins RL. Peruvian mothers' knowledge and recognition of pneumonia in children under 5 years of age. Rev Panam Salud Publica 2002; 11: 99-108.
Anh NT, Tram TT, Tri L, Huu TN, Pedersen FK, Mogensen K, Andersen E: Development of ARI case management at primary and secondary level in southern Vietnam. Southeast Asian J Trop Med Public Health 2000, 31:674-8.