Exploring The Unforeseen: Extrapulmonary tuberculosis (EPTB) With Rifampicin Resistance (Rr) In Cornelia De Lange Syndrome (Cdls) – A Rare Revelation
Abstract
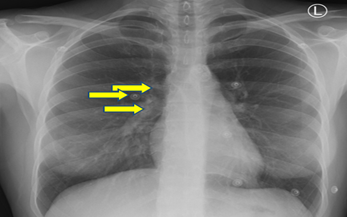
Tuberculosis (TB) remains a major global health concern, with extrapulmonary tuberculosis (EPTB) contributing significantly to its burden. This abstract discusses the clinical manifestations, diagnosis, and management of EPTB, focusing on tuberculous lymphadenitis (TBL), the most prevalent form of EPTB. Diagnostic challenges and the importance of molecular diagnostic tools like Xpert MTB/Rif Ultra are highlighted, emphasizing the need for prompt and accurate diagnosis to initiate appropriate treatment. Additionally, the abstract explores the coexistence of Cornelia de Lange syndrome (CdLS), a multisystem disorder, in a patient with EPTB with Rifampicin Resistance (RR), underscoring the complexity of managing multiple medical conditions. The significance of a multidisciplinary approach involving pediatricians, geneticists, and infectious disease specialists is emphasized in providing comprehensive care tailored to the patient's unique needs. Long-term follow-up and supportive care are crucial for optimizing outcomes in complex medical conditions like TBL and CdLS, highlighting the importance of ongoing monitoring and intervention.
Downloads
References
Global Tuberculosis Report 2022 [Internet]. [cited 2023 Aug 26]. Available from: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022
Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul) [Internet]. 2015 Apr 1 [cited 2023 Aug 26];78(2):47–55. Available from: https://pubmed.ncbi.nlm.nih.gov/25861336/
Chakaya J, Petersen E, Nantanda R, Mungai BN, Migliori GB, Amanullah F, et al. The WHO Global Tuberculosis 2021 Report – not so good news and turning the tide back to End TB. Int J Infect Dis. 2022 Nov 1;124:S26–9.
Central TBC Division. Training Module on Extrapulmonary Tuberculosis. 2023.
Gopalaswamy R, Dusthackeer VNA, Kannayan S, Subbian S. Extrapulmonary Tuberculosis—An Update on the Diagnosis, Treatment and Drug Resistance. J Respir 2021, Vol 1, Pages 141-164 [Internet]. 2021 May 26 [cited 2023 Aug 26];1(2):141–64. Available from: https://www.mdpi.com/2673-527X/1/2/15/htm
OMS. WHO consolidated guidelines on tuberculosis. Module 3: diagnosis-rapid diagnostics for tuberculosis detection,2021 update. World Heal Organ [Internet]. 2021 [cited 2023 Aug 26];Module 3:1–164. Available from: https://www.who.int/publications/i/item/9789240029415
Kline AD, Moss JF, Selicorni A, Bisgaard AM, Deardorff MA, Gillett PM, et al. Diagnosis and management of Cornelia de Lange syndrome: first international consensus statement. Nat Rev Genet 2018 1910 [Internet]. 2018 Jul 11 [cited 2023 Aug 26];19(10):649–66. Available from: https://www.nature.com/articles/s41576-018-0031-0
Kline AD, Grados M, Sponseller P, Levy HP, Blagowidow N, Schoedel C, et al. Natural history of aging in Cornelia de Lange syndrome. Am J Med Genet Part C Semin Med Genet. 2007 Aug 15;145(3):248–60.
Zumla A, Raviglione M, Hafner R, von Reyn CF. Tuberculosis. New England Journal of Medicine. 2013 Feb 21;368(8):745–55. DOI: 10.1056/NEJMra1200894
Gupta A, Mathew A. Tuberculosis lymphadenitis: A review. The Journal of Infection in Developing Countries. 2019 Oct 31;13(10):834–43. DOI: 10.3855/jidc.11768
Prasad R, Singh A, Balasubramanian VN. Extrapulmonary tuberculosis: A retrospective study of 194 cases. The Indian Journal of Tuberculosis. 2019 Jan 1;66(1):93–99. DOI: 10.1016/j.ijtb.2018.06.004
Ansari JA, Tarique M. Xpert MTB/RIF and Xpert MTB/RIF Ultra: A review of new molecular diagnostic assays for tuberculosis. International Journal of Mycobacteriology. 2018 Jan;7(1):1–6. DOI: 10.4103/ijmy.ijmy_6_18
Raizada N, Sachdeva KS, Swaminathan S, Kulsange S, Khaparde SD, Nair SA, et al. Piloting Upfront Xpert MTB/RIF Testing on Various Specimens under Programmatic Conditions for Diagnosis of TB & DR-TB in Paediatric Population. PLoS One. 2015 Oct 15;10(10):e0140375. doi: 10.1371/journal.pone.0140375. PMID: 26469691; PMCID: PMC4607299.
Bhuiyan ZA, Wahab MA. Cornelia de Lange Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535423/
Avagliano L, Bulfamante GP, Livio F, Papadia F, Maruotti GM, Pietrabissa A, et al. A comprehensive clinical and molecular approach to the diagnosis of Cornelia de Lange syndrome. Clinical Genetics. 2019 Dec;96(6):525–535. DOI: 10.1111/cge.13615
Jain A, Mondal S. Tuberculous lymphadenitis. Journal of Medical and Allied Sciences. 2014;4(1):2–10.
Sarangi S, Patra S, Sarangi R. Cornelia De Lange Syndrome: A Case Report. Scholars Journal of Medical Case Reports. 2015;3(11):1082–4.
Jackson L, Kline AD, Barr MA, Koch S. de Lange syndrome: a clinical review of 310 individuals. Am J Med Genet. 1993;47(7):940-946. doi:10.1002/ajmg.1320470709
Oliver C, Sloneem J, Hall S, Arron K. Self-injurious behavior in Cornelia de Lange syndrome: 2. Association with environmental events. J Intellect Disabil Res. 2008;52(5):451-459. doi:10.1111/j.1365-2788.2007.01004.x
Moss J, Oliver C, Berg K, Kaur G, Jephcott L, Cornish K. Prevalence of autism spectrum phenomenology in Cornelia de Lange and Cri du Chat syndromes. Am J Ment Retard. 2008;113(4):278-291. doi:10.1352/2008.113:278-291.