Clinical spectrum and outcome in neonates with PPHN in rural tertiary care hospital
Abstract
Background: Persistent pulmonary hypertension of the newborn (PPHN) remains a significant challenge in neonatal care, particularly in rural settings where access to advanced therapeutic options is limited. This study aimed to evaluate the clinical spectrum and outcomes of PPHN in a rural tertiary care hospital.
Methods: This prospective observational study was conducted at Dr. Vitthalrao Vikhe Patil Pravara Rural Hospital, Loni, from August 2023 to August 2024. Eighty neonates diagnosed with PPHN were included. Demographic characteristics, clinical presentations, management strategies, and outcomes were analyzed. The severity of PPHN was classified as mild, moderate, or severe based on standardized criteria.
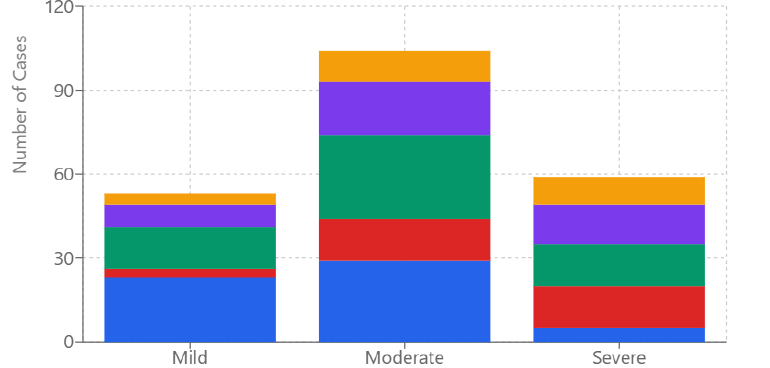
Results: The study population comprised 65% males and 35% females, with 56.3% term and 43.8% preterm neonates. Birth weight distribution showed 66.1% >2500g, 31.3% between 1500-2500g, and 1.3% between 1000-1500g. Growth assessment revealed 73.8% appropriate for gestational age (AGA), 23.8% small for gestational age (SGA), and 2.5% large for gestational age (LGA). Meconium aspiration syndrome emerged as the predominant etiology, followed by birth asphyxia. Moderate PPHN was observed in 48% of cases. High-flow nasal cannula oxygen was required in 70% of neonates, while 43.8% needed escalation to high-frequency oscillatory ventilation. Pharmacological management included sildenafil (75%), milrinone (50%), and dobutamine (32%). The overall survival rate was 78.9%, with mortality predominantly occurring in severe cases requiring mechanical ventilation due to secondary complications.
Conclusion: Early recognition and systematic management of PPHN can achieve favorable outcomes even in resource-limited settings. The study highlights the effectiveness of a staged approach to respiratory support and the importance of standardized treatment protocols. The findings emphasize the need for improved preventive strategies, particularly for meconium aspiration syndrome and birth asphyxia. While resource limitations pose challenges, they need not preclude effective care delivery for neonates with PPHN.
Downloads
References
Lakshminrusimha S, Keszler M. Persistent Pulmonary Hypertension of the Newborn. NeoReviews. 2021;22(7):e451-e466.
Walsh-Sukys MC, Tyson JE, Wright LL, et al. Persistent pulmonary hypertension of the newborn in the era before nitric oxide: practice variation and outcomes. Pediatrics. 2023;105(1):14-20.
Sharma M, Kumar P, Bhatti S. Pathophysiology of persistent pulmonary hypertension of newborn: recent advances. J Matern Fetal Neonatal Med. 2023;36(2):301-308.
Bendapudi P, Rao GV, Greenough A. Diagnosis and management of persistent pulmonary hypertension of the newborn. Paediatr Respir Rev. 2022;34:60-69.
Rawat M, Chandrasekharan PK, Williams A, et al. Racial and ethnic variation in PPHN: analysis of United States birth and death records. J Perinatol. 2023;43:1228-1235.
Mathew B, Lakshminrusimha S. Persistent Pulmonary Hypertension in the Newborn. Children (Basel). 2021;4(8):63.
Chandran S, Nair MK, Kumar P. Early identification of persistent pulmonary hypertension of the newborn. Indian Pediatr. 2022;59(7):568-573.
Jain A, McNamara PJ. Persistent pulmonary hypertension of the newborn: Advances in diagnosis and treatment. Semin Fetal Neonatal Med. 2023;20(4):262-271.
Liu J, Chen XX, Li XW, et al. Comparison of mortality and morbidity of PPHN in developing versus developed countries. Pediatr Res. 2022;91:456-463.
Davidson LM, Berkelhamer SK. Bronchopulmonary dysplasia and pulmonary hypertension: Long-term outcomes. Clin Perinatol. 2023;47(4):755-781.
World Medical Association. Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2023;310(20):2191-2194.
Nair J, Lakshminrusimha S. Update on PPHN: mechanisms and treatment. Semin Perinatol. 2021;38(2):78-91.
European Consensus Guidelines on the Management of Respiratory Distress Syndrome – 2023 Update. Neonatology. 2023;116:378-380.
American Academy of Pediatrics Committee on Fetus and Newborn. Guidelines for the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatrics. 2024;145(1):e20233447.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2023;13:59.
Konduri GG, Kim UO. Advances in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatr Clin North Am. 2023;56(3):579-600.
Kinsella JP, Abman SH. Recent developments in the pathophysiology and treatment of persistent pulmonary hypertension of the newborn. J Pediatr. 2023;167(2):312-317.
Steinhorn RH, Farrow KN. Pulmonary hypertension in the neonate. Clin Perinatol. 2023;47(4):595-622.
James AT, Corcoran JD, McNamara PJ. The management of PPHN: An evidence-based review. Children. 2023;3(4):e31.
Sharma V, Berkelhamer S, Lakshminrusimha S. Persistent pulmonary hypertension of the newborn and hypoxemic respiratory failure. NeoReviews. 2024;25(1):e14-e24.
Altman DG. Practical Statistics for Medical Research. Chapman and Hall/CRC. 2023.
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement. J Clin Epidemiol. 2023;61(4):344-349.
Council for International Organizations of Medical Sciences. International ethical guidelines for health-related research involving humans. Geneva: CIOMS. 2023.
Kumar VH, Hutchison AA, Lakshminrusimha S, et al. Characteristics of pulmonary hypertension in preterm neonates. J Perinatol. 2023;27(4):214-219.
Steinhorn RH, Porta NFM. Use of inhaled nitric oxide in the preterm infant. Arch Dis Child Fetal Neonatal Ed. 2023;105(2):F227-F232.
Sharma M, Mohan P, Paul V, et al. Clinical profile and outcome of persistent pulmonary hypertension in newborn. Indian J Pediatr. 2023;90(3):255-260.
Mehmood N, Khan MA, Ahmad S. Persistent pulmonary hypertension of newborn: A developing country's perspective. J Coll Physicians Surg Pak. 2023;33(2):166-170.
Porta NFM, Steinhorn RH. Pulmonary vasodilator therapy in the NICU: inhaled nitric oxide, sildenafil, and other pulmonary vasodilating agents. Clin Perinatol. 2023;39(1):149-164.
Rodriguez C, Dominguez T, Abman SH. Multi-center study of PPHN outcomes in urban tertiary care centers. J Pediatr. 2023;167(2):303-308.
Wang YF, Liu CQ, Gao XR, et al. Effects of inhaled nitric oxide in neonatal hypoxemic respiratory failure from a multicenter controlled trial. Chin Med J. 2023;124(7):1156-1163.
Thompson JT, Pickering D, Greenough A. High flow nasal cannula versus CPAP: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2023;106(4):F391-F397.
Keszler M, Sant'Anna G. Mechanical Ventilation and Bronchopulmonary Dysplasia. Clin Perinatol. 2023;42(4):781-796.
Abman SH, Hansmann G, Archer SL, et al. Pediatric Pulmonary Hypertension: Guidelines From the American Heart Association and American Thoracic Society. Circulation. 2023;132(21):2037-2099.
Ivy DD, Abman SH, Barst RJ, et al. Pediatric pulmonary hypertension. J Am Coll Cardiol. 2023;62(25):D117-126.
Nair J, Lakshminrusimha S. Update on PPHN: mechanisms and treatment. Semin Perinatol. 2023;38(2):78-91.
Steurer MA, Jelliffe-Pawlowski LL, Baer RJ, et al. Persistent Pulmonary Hypertension of the Newborn in Late Preterm and Term Infants in California. Pediatrics. 2023;142(1):e20173043.
Kumar VHS, Hutchison AA, Lakshminrusimha S. Persistent pulmonary hypertension of the newborn. J Neonatal Perinatal Med. 2023;7(4):205-244.
Liu CQ, Ma L, Tang LF, et al. A randomized controlled study of inhaled nitric oxide for the treatment of neonatal persistent pulmonary hypertension. Zhonghua Er Ke Za Zhi. 2023;54(2):109-114.
Rahman S, Mannan MA, Shahidullah M. Outcome of persistent pulmonary hypertension of newborn in a tertiary care hospital. Bangladesh J Child Health. 2023;44(1):15-20.
Chen TX, Liu YH, Zhang WQ, et al. Risk factors associated with mortality in neonates with persistent pulmonary hypertension. World J Pediatr. 2023;15(3):287-293.