Did chess players have better mental state amidst the pandemic? - An assessment through the DASS index among Indians
Abstract
Background and Aim: The Covid 19 pandemic has created the most vulnerable health situation, forcing it to change the lives of billions. The main aim of this study is to evaluate the difference in mental health conditions between a chess-playing and non-chess-playing (control) group to determine the positive impacts of the game.
Methods: 400 participants were selected for the study (cases=100, controls=300) during the second wave of Covid-19 in India. An individual with a record of playing chess was included in the case group, while anyone who does not play chess was chosen as the control. This was a voluntary study wherein self-administered google forms were used as questionnaires to obtain data. Internal consistency, categorical analysis using Pearson Chi-Square Test at 95% confidence, t-test for the mean difference of DASS scores, and odds ratio at 95% confidence intervals were assessed.
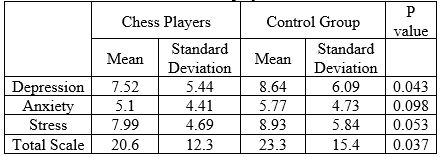
Results: Internal consistency of the DASS index was high, with Cronbach's alphas of 0.9103 and 0.9443, respectively, for the chess-playing and control groups. Categorical analysis revealed that regularity and intensity had no association in alleviating mental health situations but reduced the risk of mental health deterioration among chess players (OR= 0.3628; 95% CI 0.166-0.789). Independent t-tests revealed significantly lower DASS scores for the chess-playing group concerning depression and total DASS index.
Conclusion: This study has generated preliminary evidence and calls for further research to understand the extent of this positive outcome. Enough evidence in this regard would appeal to the popularization and extensive coverage of chess.
Downloads
References
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, Abbasi-Kangevari M, Abbastabar H, Abd-Allah F, Abdelalim A, Abdollahi M. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020 Oct 17;396(10258):1204-22.
Sagar R, Dandona R, Gururaj G, Dhaliwal RS, Singh A, Ferrari A, Dua T, Ganguli A, Varghese M, Chakma JK, Kumar GA. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. The Lancet Psychiatry. 2020 Feb 1;7(2):148-61.
Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain, behavior, and immunity. 2020 Jul;87:49.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The lancet. 2020 Mar 14;395(10227):912-20.
Bloom DE, Cafiero-Fonseca ET, Candeias V, Adashi E, Bloom L, Gurfein L, Jané-Llopis E, Lubet A, Mitgang E, Saxena A. Economics of non-communicable diseases in India: the costs and returns on investment of interventions to promote healthy living and prevent, treat, and manage NCDs. InWorld economic forum, Harvard school of Public Health 2014 (pp. 22-23).
Casey P, Dowrick C, Wilkinson G. Adjustment disorders: fault line in the psychiatric glossary. The British Journal of Psychiatry. 2001 Dec;179(6):479-81.
Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. Psychology Foundation of Australia; 1996.
Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. Journal of abnormal psychology. 1991 Aug;100(3):316.
Lovibond SH, Lovibond PF. Overview of the DASS and its uses. Available from: www2. psy. unsw. edu. au/Groups/Dass/over. htm. Accessed February. 2009;15.
Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological assessment. 1998 Jun;10(2):176.
Bottesi G, Ghisi M, Altoè G, Conforti E, Melli G, Sica C. The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Comprehensive psychiatry. 2015 Jul 1; 60:170-81.
Tonsing KN. Psychometric properties and validation of Nepali version of the Depression Anxiety Stress Scales (DASS-21). Asian Journal of Psychiatry. 2014 Apr 1; 8:63-6.
Vasconcelos-Raposo J, Fernandes HM, Teixeira CM. Factor structure and reliability of the depression, anxiety and stress scales in a large Portuguese community sample. The Spanish Journal of Psychology. 2013;16.
Hänggi, J., Brütsch, K., Siegel, A. M., & Jäncke, L. (2014). The architecture of the chess player׳ s brain. Neuropsychologia, 62, 152-162.
Grabner RH, Stern E, Neubauer AC. Individual differences in chess expertise: A psychometric investigation. Acta psychologica. 2007 Mar 1;124(3):398-420.
Fattahi F, Geshani A, Jafari Z, Jalaie S, Mahini MS. Auditory memory function in expert chess players. Medical Journal of the Islamic Republic of Iran. 2015; 29:275.
Sala G, Gobet F. Does far transfer exist. Negative evidence from chess, music, and working memory training. Curr Dir. 2017.
Lillo-Crespo M, Forner-Ruiz M, Riquelme-Galindo J, Ruiz-Fernández D, García-Sanjuan S. Chess practice as a protective factor in dementia. International Journal of Environmental Research and Public Health. 2019 Jan;16(12):2116.
Coyle JT. Use it or lose it—do effortful mental activities protect against dementia? New England Journal of Medicine. 2003 Jun 19;348(25):2489-90.
Fuentes JP, Villafaina S, Collado-Mateo D, de la Vega R, Gusi N, Clemente-Suárez VJ. Use of biotechnological devices in the quantification of psychophysiological workload of professional chess players. Journal of Medical Systems. 2018 Mar;42(3):1-6.
Grau-Pérez G, Moreira K. A study of the influence of chess on the Executive Functions in school-aged children. Studies in Psychology. 2017 May 4;38(2):473-94.
Radtke EL, Düsing R, Kuhl J, Tops M, Quirin M. Personality, stress, and intuition: Emotion regulation abilities moderate the effect of stress-dependent cortisol increase on coherence judgments. Frontiers in psychology. 2020 Feb 27; 11:339.