Postprandial lipid profile abnormalities in Type 2 Diabetes Mellitus
Abstract
Background: Dyslipidemia is commonly seen as diabetes. Type 2 DM is one of the most common secondary causes of hyperlipidemia. Type 2 diabetes mellitus is associated with the development of premature arteriosclerosis and higher cardiovascular morbidity and mortality. Diabetic dyslipidemia is believed to play an important role in the pathogenesis of accelerated atherosclerosis in this condition. The predominant lipid abnormalities seen in diabetes mellitus are an elevated serum triglyceride (Tg) level and a low HDL-C level. While several studies have found a significant association of fasting hypertriglyceridemia and coronary artery disease (CAD) in diabetes mellitus, the relationship is not consistent particularly after adjusting for fasting HDL-C Levels.9 It is being increasingly believed that atherosclerosis is a postprandial phenomenon as at least with respect to lipids, we are in the postprandial phase for nearly 2/3rd of the day. High postprandial triglycerides have shown a strong and independent association with CAD. Earlier studies of postprandial lipids in diabetes mellitus have suggested abnormalities of Tg metabolism secondary to insulin resistance (15) although results have not been consistent.
Aims: To assess the postprandial lipid abnormalities in type 2 diabetic patients attending PRH Loni.
Objective: To study postprandial lipid profile abnormalities in Type 2 diabetes patients as compared to non diabetics.
Methodology: The present study was a prospective case-control type of study that was conducted in Pravara Rural Hospital, Loni. (PRH) with a sample size of 187 (137 cases and 50 controls).
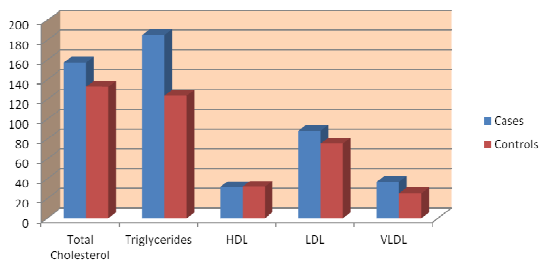
Results: The mean age of cases was 57.78 ±12.79 years and of controls was 60.50 ±14.39 years. The fasting bsl in cases was 204.61 ±105.01mg/dl and controls were 98.52±30.03 mg/dl. Postprandial bsl was 235.13 ±114.85 mg/dl in cases and 141.92 ±62.47 mg/dl in controlsPhadke C. & (P= 0.0001; P<0.05 is significant). Total cholesterol level in cases was 157.52 ±53.08 mg/dl and in controls was133.06 ±34.22 (P=0.002). Triglycerides level was 185.23 ±104.34 mg/dl in cases and 123.70 ±47.83 mg/dl in controls (P=0.0001). VLDL value in cases was 37.14 ±21.41mg/dl and in controls was 25.14 ±10.46mg/dl (P=0.0002).
Downloads
References
Powers Alvin C. Harrison's Principles of Internal Medicine 19th Edition; 2399
Alvin C. P. Screening for Type 2 Diabetes in Diabetic care. ADA. Jan 2004;27(1):11–14
Harold EL. Type 2 Diabetes Mellitus: An overview. Clinical Chemistry. 1999;45(8):1339–45.
Maeda E, Yoshino G, Kasuga M. Diabetes mellitus as a risk factor for arteriosclerosis. Nippon Rinsho. 1993 Aug;51(8):2170–76
Ushuizen MF, Diamant M, Heine RJ. Postprandial dysmetabolism and cardiovascular disease in Type 2 Diabetes. Postgrad Med J. 2005;81:1–6
Tentolouris N, Stylianou A, Lourida E, Perrea D, et al. High postprandial triglyceridemia in patients with Type 2 Diabetes and microalbuminuria. Journal of Lipid Research. 2007;48:218–25
Axelsen M, Smith U, Eriksson JW, Jansson PA, et al. Postprandial Hypertriglyceridemia and Insulin Resistance in Normoglycemic First-Degree Relatives of Patients with Type 2 Diabetes. Ann Intern Med. 1999;131:27–31
Evans M, Anderson RA MB, Graham J, Gethin R, et al. Ciprofibrate therapy Improves Endothelial Function and Reduces Postprandial Lipemia and Oxidative Stress in Type 2 Diabetes Mellitus. Circulation. 2000;101:1773–79
Annuzzi G, Natale CD, Iovine C, Patti L, Rivellese A, et al. Insulin resistance is independently associated with postprandial Alterations of triglyceride-rich ipoproteins in Type 2 Diabetes Mellitus. Arterioscler Thromb Vasc Biol. 2004;24:2397–402
Ferreira AC. Postprandial hypertriglyceridemia increases circulating levels of endothelial cell Microparticles. Circulation. 2004;110:3599–603.
Lewis GF, O’Meara NM, Soltys PA, Blackman JD, Iverius PH, Pugh WL, Getz GS, Polonsky KS. Fasting Hypertriglyceridemia in non-insulin dependent diabetes mellitus is an important predictor of postprandial lipid and lipoprotein abnormalities. J Clin Endocrinol Metab 1991;72:934-44
Chen YD, Swami S, Skowronski R, Coulston A, Reaven GM. Differences in postprandial lipemia between patients with normal glucose tolerance and non-insulin dependent diabetes mellitus. J Clin Endocrinol Metab 1993;76:172-77.
American Diabetes Association. Diabetes facts and figures. 2016. http://www.diabetes.org/diabetesstatistics.jsp.
American Diabetes Association. Standards for medical care in diabetes 2007. Diabetes Care 2016; 30(Suppl 2):S62–S73.
American Diabetes Association. Standards for medical care in diabetes. Diabetes Care. 2017; 30 (1): 4–41.
Kahn SE, Porte D Jr. The pathophysiology of type II (non-insulin dependent) diabetes mellitus: Implications for treatment. In: Porte D Jr, Sherwin RS, eds. Ellenberg& Rifkin’s Diabetes Mellitus, 5th ed. Stamford, CT: Appleton & Lange. 1997:487–512.
American Diabetes Association. Gestational diabetes mellitus. Diabetes Care 2004; 27 (1): 88–90.
A Ramachandran, AK Das et al. Current Status of Diabetes in India and Need for Novel Therapeutic Agents supplement to JAPI 2010; 58: 7-9.