Spectrum of clinicopathological and biochemical variations among severe plasmodium vivax malaria cases: a vision from eastern India
Abstract
Background: Plasmodium vivax (P. vivax) is geographically widely distributed with up to 2.5 billion people at risk and an estimated 70-80 million cases every year. India contributes 77% of total malaria in Southeast Asia. Retrospective analysis of the burden of malaria showed that disability-adjusted life years due to malaria were 1.86 million years. According to a recent study, West Bengal contributes 11% of total malaria cases in the country.
Aim and objective: This study tends to focus on severe and non-severe vivax malaria, the complications and outcome of P. vivax malaria infections as there is very limited information on age- and sex-specific seasonal prevalence of malaria in different paradigms in the country with most of the point prevalence studies in India have been carried out for outbreak/epidemic investigations.
Materials and Methods: A hospital-based prospective study was conducted over a period of one and half years in a medical college and hospital comprising of 138patients with fever (≥37.5˚C), peripheral smear, and/or rapid diagnostic tests positive for P. vivax. Previously established cases of CKD, hematological abnormalities, chronic liver diseases, neuropsychiatric disorders were excluded from our study. Demographical, clinical and laboratory parameters including liver function test, renal function test were documented and were presented in tabular, graphical, and statistical means.
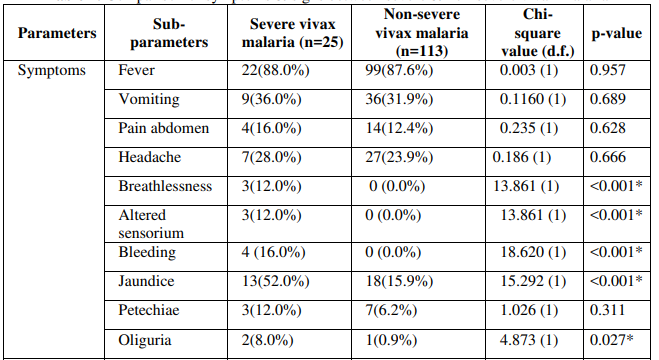
Observation and Results: 138 hundred patients were taken up for the study, which included males and females. The majority of the patients were in the second decade. Jaundice was present in 22% of patients and vomiting in 32% of the patients. Hepatomegaly was seen in 16 % of cases and 33% of cases had splenomegaly. ARDS was seen in 16% of severe malaria cases. Acute kidney injury was seen in 8% and cerebral malaria was seen in 12 % of severe malaria cases. Multi-organ dysfunction has seen in12 % of cases. There was 1 death in the study due to multi-organ dysfunction.
Conclusion: Life-threatening complications such as ARDS, AKI, cerebral malaria, and MODS can be seen in P. vivax mono infections.
Downloads
References
Garcia LS. Malaria. Clinics in Laboratory Medicine. 2010; 30: 93-129.
Guidelines for diagnosis and treatment of malaria nvbdcp 2011
WHO. World Malaria report 2011.
Ric NP, Emiliana T, Carlos AG, Shunmay Y, Nicholas JW, Nicholas M. Vivax Malaria neglected and not benign. American journal of tropical medicine and hygiene.2007; 77:79- 87.
Price RN, Douglas NM, Ansteya NM. New developments in Plasmodium vivax malaria: severe disease and the rise of chloroquine resistance. Current opinion in infectious diseases.2009; 22: 430-35.
Bhattacharjee P, Dubey S, Gupta VK, Agarwal P, Mahato MP. The clinicopathologic manifestations of plasmodium vivax malaria in children: A growing menace. Journal of Clinical and Diagnostic Research.2013; 7: 861-67.
WHO. World Malaria report 2013 8. Farogh A, Qayyum A, Haleem A and Ghaffar A. Haematological abnormality in malaria. Biomedica vol.25,JanJun.2009/Bio-10.Doc.p.52-55
Muddaiah M, Prakash Ps. A study of clinical profile of malaria in a tertiary referral centre in South Canara. J Vector Borne Dis 2006 mar; 43(1); 29-33
Bashawri LAM, Mandil AA, Bahanassy AA and Mirghani AA. Malaria: Haematological aspects. Annals of Saudi medicine 2002 (22): no5-6.p.372-76.
Jadhav UM, Patkar VS, Kadam NN. Thrombocytopenia in Malaria – Correlation with type and severity of Malaria .JAPI 2007; 52: 615-18.