Quality Improvement project for management of Depression in Chronic Kidney Disease patients receiving haemodialysis
Abstract
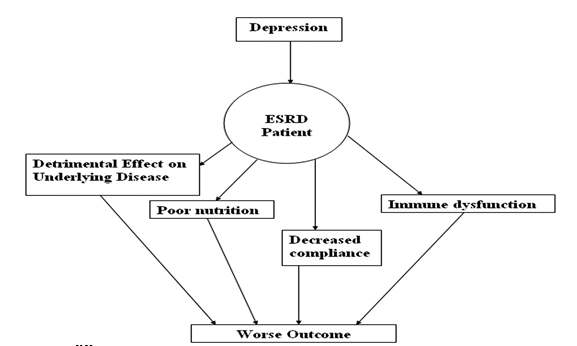
Aim: To apply quality improvement methodology and apply a few appropriate interventions to reduce the prevalence of depression. The NICE guidelines 2009 for depression management were used to guide the introduction of appropriate interventions. PHQ-9 was used to score depression before and after the intervention. The interventions included painting and decorating the unit in bright colors, adding a television facility, taking strict measures for maintaining cleanliness, allowing one attendant per patient inside the unit, making few quiet corners if the patient intends to sleep during the session. Methods: Diagrams, flowcharts were used to show aims and objectives. A PDSA cycle (Plan, Do, Study, Act) was used. The prevalence of depression in dialysis patients was calculated using the PHQ-9 questionnaire. A new plan for the dialysis department decoration and introduction of facilities was formulated with input from the dialysis department staff; including the nurses, technical staff, and the in-charge of the Nephrology Department. Results: 120 patients involved in the dialysis sessions were targeted in this project for the six months duration from April 2018-Sep 2018.40% of the patients (48) were found to be suffering from moderate-moderately severe depression (score range 10-19) via the filled PHQ-9 questionnaire. Four months after the introduction of various changes the PHQ-9 was filled by the same patients. Now the prevalence of depression reduced to 10% (12). Also, the patient's still scored as being depressed were in the mild depression range(i.e. score on PHQ:5-9). Conclusion: Following the implementations especially focusing on the counseling sessions (as mentioned in NICE guidelines)and increasing the Doctor's availability in the department with some environmental changes, there was an improvement in overall patient care. Especially the patient's mental health improved and the overall mood of the patient was elevated. different facilities introduced along with the changes in the overall look of the department and focusing on patient's mental health improvement by counseling and improved interaction of patients with their care providers like junior doctors helped a lot.
Downloads
References
National Kidney Foundation. 2020. Facts About Chronic Kidney Disease. [online] Available at: http://www.kidney.org/atoz/content/about-chronic-kidney-disease> [Accessed 5 August 2020].
<https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3130152/. n.d. . Quality Of Life In Patients With Chronic Kidney Disease
Akman, B., Uyar, M., Afsar, B., Sezer, S., Nurhan Ozdemir, F. and Haberal, M., 2007. Adherence, depression and quality of life in patients on a renal transplantation waiting list. Transplant International, 20(8), pp.682-687.
Santacruz, J., Alonso Babarro, A., García Llana, H., Del Peso Gilsanz, G., Sánchez Villanueva, R., Bajo Rubio, M., Castillo Plaza, A. and Selgas Gutierrez, R., 2018. FP659QUALITY OF LIFE AND SURVIVAL IN PATIENTS WITH STAGE 5 CHRONIC KIDNEY DISEASE IN DIALYSIS VERSUS CONSERVATIVE TREATMENT. Nephrology Dialysis Transplantation, 33(suppl_1), pp.i267-i267.
Nabolsi, M., Wardam, L. and Al-Halabi, J., 2013. Quality of life, depression, adherence to treatment, and illness perception of patients on hemodialysis. International Journal of Nursing Practice, 21(1), pp.1-10.
Mujais, S., Story, K., Brouillette, J., Takano, T., Soroka, S., Franek, C., Mendelssohn, D., and Finkelstein, F., 2009. Health-related Quality of Life in CKD Patients: Correlates and Evolution over Time. Clinical Journal of the American Society of Nephrology, 4(8), pp.1293-1301.
2020. [online] Available at: [Accessed 5 August 2020].
2020. [online] Available at: <https://pubmed.ncbi.nlm.nih.gov/23486521/> [Accessed 5 August 2020].
Nimh.nih.gov. 2020. NIMH » Older Adults And Depression. [online] Available at: <https://www.nimh.nih.gov/health/publications/older-adults-and-depression/index.shtml> [Accessed 5 August 2020].
Spitzer, R., 2020. Validation And Utility Of A Self-Report Version Of PRIME-MDThe PHQ Primary Care Study. 2020. [online] Available at: <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3797653/> [Accessed 5 August 2020].
Institute For Healthcare Improvement. Driver Diagram. [internet]. 2017.[cited 21st September 2017]. Avalible from http://www.ihi.org/resources/Pages/Tools/Driver- Diagram.aspx.
Pathways.nice.org.uk. 2020. Depression - NICE Pathways. [online] Available at: <http://pathways.nice.org.uk/pathways/depression> [Accessed 5 August 2020].
PDSA: Plan-Do-Study-Act (Rapid Cycle Improvement) - Minnesota Dept. of Health 2019, State.mn.us.
Clinical Management of Depression - Summary of RANZCP Guidelines 2019, Psych Scene Hub, viewed 23 August 2019, <https://psychscenehub.com/psychinsights/clinical-management-depression-summary-ranzcp-guidelines/>.
ABRAM, HS, MOORE, GL & WESTERVELT, FB 1971, ‘Suicidal Behavior in Chronic Dialysis Patients’, American Journal of Psychiatry, vol. 127, no. 9, pp. 1199–1204.
Shirazian, S, Grant, CD, Aina, O, Mattana, J, Khorassani, F & Ricardo, AC 2017, ‘Depression in Chronic Kidney Disease and End-Stage Renal Disease: Similarities and Differences in Diagnosis, Epidemiology, and Management’, Kidney International Reports, vol. 2, no. 1, pp. 94–107
CKD Patients Aren’t Having Mental Health Needs Fully Met 2020, www.medpagetoday.com, viewed 5 August 2020, <https://www.medpagetoday.com/meetingcoverage/nkf/85671>.
NHS Choices 2019, Treatment-Chronic kidney disease. https://www.nhs.uk/conditions/kidney-disease/treatment/
Gilman, SE, Sucha, E, Kingsbury, M, Horton, NJ, Murphy, JM & Colman, I 2017, ‘Depression and mortality in a longitudinal study: 1952–2011’, Canadian Medical Association Journal, vol. 189, no. 42, pp. E1304–E1310.
Koo, J-R, Yoon, J-Y, Joo, M-H, Lee, H-S, Oh, J-E, Kim, S-G, Seo, J-W, Lee, Y-K, kim, H-J, Noh, J-W, Lee, S-K & Son, B-K 2005, ‘Treatment of Depression and Effect of Antidepression Treatment on Nutritional Status in Chronic Hemodialysis Patients’, The American Journal of the Medical Sciences, vol. 329, no. 1, pp. 1–5