Climate change: A potential risk factor for cancer?
Abstract
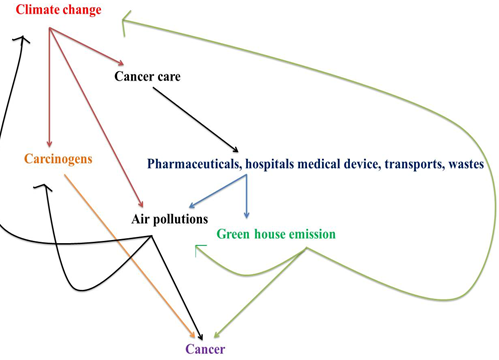
Cancer, mainly known for abnormal growth and altered cellular function is now the second prominent reason of death in the world. There are so many factors responsible for this disease and one of the major factors in climate change. The deviations of weather patterns that are definitely a result of human activities over long periods of time generally referred to as climate change. The consequences include increasing temperature, melting of ice, rising sea levels, increasing wind speed, changes in rainfall patterns, etc. Due to all these concerns, the most important resource for a healthy life– Air, Water, and Food are gets disturbed and as a result, causes several health-related problems. Previous researches related to this field also demonstrated that climate change played a critical role in cancer risk and cancer surveillance. It increases the number of carcinogens and also blocks patients’ access to cancer hospitality. Here in this article, you will get to know about the impacts of climate changes on health. Why this can be potential risk factors for cancer by focusing mainly on lung and skin cancer and about some well-known limitations that we need have to resolve in the near future. In this concern, several steps have been implicated globally but more preparedness and attentiveness are reasonable.
Downloads
References
Haines A, Kovats RS, Campbell-lendrum D, Corvalan C. Climate change and human health : Impacts , vulnerability and public health *. 2006:585-596. doi:10.1016/j.puhe.2006.01.002
Wright CY, Norval M, Kapwata T, et al. The Incidence of Skin Cancer in Relation to Climate Change in South Africa. :1-11.
Asia S, World TS, Assembly H, States M, Region TSEA, Meeting T. Climate Change and Health. 2008;2.
Kaffenberger BH, Shetlar D, Mph SN, Rosenbach M. The effect of climate change on skin disease in North America. J Am Dermatology. 2016. doi:10.1016/j.jaad.2016.08.014
Bharath AK. Impact of climate change on skin. 2009:215-218. doi:10.1258/jrsm.2009.080261
https://www.hsph.harvard.edu/c-change/news/climate-change-and-cancer/.
Nogueira LM. Climate Change and Cancer. 2020;70(4):239-244. doi:10.3322/caac.21610
Johnson H, Kovats RS, McGregor GR et al. The impact of the 2003 heatwave on mortality and hospital admissions in England. Heal Stat Q. 2005:6-11.
Giang, P. N., Dung, d., Bao Giang, K., Vinhc, H. V., & Rocklöv J. The effect of temperature on cardiovascular disease hospital admissions among elderly people in Thai Nguyen Province, Vietnam. Glob Health Action. 2014;(7):23649.
Ahern M, Kovats RS, Wilkinson P, Few R MF. Global health impacts of floods: epidemiologic evidence. Epidemiol Rev. 2005:36-46.
Albering HJ, van Leusen SM, Moonen EJC HJ, JCS K. Human health risk assessment: a case study involving heavy metal soil contamination after the flooding of the river Meuse during the winter of 1993–1994. Env Heal Perspect. 1999:37–43.
Meusel D KWL learned from the 2002 flood in, Dresden, German.In: Menne B, Bertollini R, Kirch W editors. Extreme weather events and public health response. Berlin. Springer. 2005:175–84.
Kovats S, Bouma MJ, Hajat S, Worrell E HA. El Nino and health. Lancet. 2003:1481–1489.
International Agency for Research on Cancer. Polychlorinated Dibenzo-para- Dioxins and polychlorinated dibenzofurans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 69. World Health Organization/International Agency for Research on. World Heal Organ Agency Res Cancer;. 2020. iarc.fr/87.
Liu JC, Mickley LJ, Sulprizio MP et al. Particulate air pollution from wildfires in the Western US under climate change. Clim Chang. 2016;(138):655-666.
Jaffe D, Hafner W, Chand D WA, D. S. Interannual variations in PM2.5 due to wildfires in the Western United States. 2008;(42):2812-2818.
Battilani P, Toscano P V der F-K, HJ et al. Aflatoxin B1 contamination in maize in Europe increases due to climate change. Sci Rep. 2016;6:24328.
A.A. Motalebi, K. Ardalani and S. Jamili. Effect of Temperature on the Produced Aflatoxins in the Rainbow Trout Feed in West Azerbaijan Province. J Fish Aquat Sci. 2008;3(6):pp392-397.
Diffey B. Climate change, ozone depletion and the impact on ultraviolet exposure of human skin. Phys Med Biol. 2004;49:R1-R11.
Narayanan, D.L.; Saladi, R.N.; Fox JL. Ultraviolet radiation and skin cancer. Int J Dermatol. 2010;49:978–986.
Corona R, Dogliotti E, D’Errico M et al. Risk factors for basal cell carcinoma in a Mediterranean population: role of recreational sun exposure early in life. Arch Derm. 2001;137:1162-1168.
Ziegler A, Jonason AS, Leffell DJ et al. Sunburn and p53 in the onset of skin cancer. Nature. 1994;372:773-776.
Mancebo, S.E.; Wand SQ. Recognizing the impact of ambient air pollution on skin health. J Eur Acad Dermatol Venereol. 2015;29:2326–2332.
Zegarska, B.; Pietkun, K.; Giemza-Kucharska, P.; Zegarski, T.; Nowacki, M.S.; Romanska-Gocka K. Changes in Langerhans cells during skin ageing. Postep Dermatol Alergol. 2017;34:260–267.
Ku N. Commentary : Abating climate change and lung cancer ! 2011;(March):729-730. doi:10.1093/ije/dyr037
Hopkinson NS, Hart N, Jenkins G, et al. Climate change and lung health : the challenge for a new president. 1985:295-296. doi:10.1136/thoraxjnl-2017-209978
Zhang JJ SK. Household air pollution from coal and biomass fuels in China: measurements, health impacts, and interventions. Env Heal Perspect. 2007;115:8848-8855.
Torres-Duque C, Maldonado D, Perez-Padilla R EM, G. V. Biomass fuels and respiratory diseases: a review of the evidence. Proc Am Thorac Soc. 2008;5:577-590.
Kurmi OP, Semple S, Simkhada P, Smith WC AJ. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65:221-228.
Lan Q, Chapman RS, Schreinemachers DM, Tian L HX. Household stove improvement and risk of lung cancer in Xuanwei, China. J Natl Cancer Inst. 2002;94:826-835.
https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health.
https://www.india.gov.in/spotlight/pradhan-mantri-ujjwala-yojana#tab=tab-1.
Man RX, Lack DA, Wyatt CE M V. The effect of natural disasters on cancer care: a systematic review. Lancet Oncol. 2018;19:e482-e499.
Nogueira LM, Sahar L EJ, Jemal A YK. Association between declared hurricane disasters and survival of patients with lung cancer undergoing radiation treatment. JAMA. 2019;322:269-271.
FDA UF and DA, Scott NRFC, Gottlieb MD. updates on some ongoing shortages related to IV fluids. US Food and Drug Administration; 2020. fda.gov/news-event s/%0Apress -annou nceme nts/fda-commi ssion%0Aer-scott -gottl ieb-md-updat es-some-ongoi%0Ang-short ages-relat ed-iv-fluids.
MacNeill AJ, Lillywhite R BC. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Heal. 2017:e381-e388.
Chung JW MD. Estimate of the carbon footprint of the US health care sector. JAMA. JAMA. 2009;302:1970-1972.
Demark-Wahnefried W. Cancer survival: time to get moving? Data accumulate suggesting a link between physical activity and cancer survival. J Clin Oncol. 2006;24:3517-3518.
Monninkhof EM, Elias SG VF, Al. E. Physical activity and breast cancer: a systematic review. Epidemiology. 2007;18:137-157.