Iron with folic acid supplemenation and birth weight in Ethiopia: Systemic review and meta-analysis
Abstract
Objective: The aim of this systemic review and meta-analysis was to examine the relationship between iron with folic acid supplementation and low birth weight in Ethiopia Previous studies on iron with folic acid supplementation and low birth weight indicated different findings. We include 24 studies in different regions of Ethiopia. We have done this study focusing on iron with folic acid supplementation.
Materials and Methods The databases searched were PUBMED and Advanced Google Scholar. on reference manager software reporting iron with folic acid supplementation and low birth weight. Three researchers have carried out the data extraction and assessed independently the articles for inclusion in the review using the risk-of-bias tool guided by the PRISMA checklist.
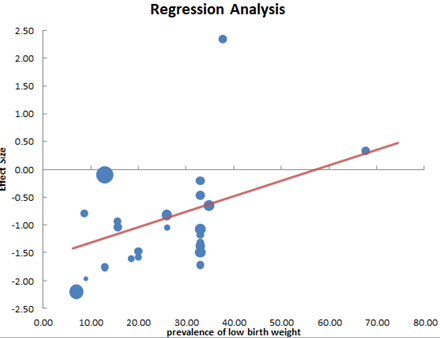
Results: Twenty-four observational studies involving 10989 participants, 2348 newborns have low birth weight were included. The combined effect size (OR) for low birth weight r comparing women who have an iron with folic acid supplementation versus women who did not have an iron with folic acid supplementation was 0.37 (95%CI 0.25 to 0.55), p<0.00001, I2 = 91 %). There was significant heterogeneity. No publication bias was observed, women reported iron with folic acid supplementation during current pregnancy in all studies, the proportion of low birth weight among women who reported iron with folic acid supplementation during the current pregnancy was 1392 (17.85%).
Conclusions: Women who take iron with folic acid supplementation during pregnancy have a 67% decreased in delivering low birth weight newborns in Ethiopia.
Downloads
References
UNICEF: Low Birth Weight New York, USA: United Nations Children’s Fund; 2001
P. Bharati, M. Pal, M. Bandyopadhyay, A. Bhakta, S. Chakraborty, and P. Bharati, “Prevalence and causes of low birth weight in India,” Malaysian Journal of Nutrition, vol. 17, no. 3, pp. 45–56, 2011
Demelash H, Motbainor A, Nigatu D, Gashaw K, Melese A. Risk factors for low birth weight in Bale zone hospitals, South-East Ethiopia: a casecontrol study. BMC Pregnancy Childbirth. 2015; 15:264
Zeleke BM, Zelalem M, Mohammed N. Incidence and correlates of low birth weight at a referral hospital in Northwest Ethiopia. Pan Afr Med J. 2012;12(1):4
WHO guide lineon optimal feeding of low birth weight in low and middile income countries. Geneva, World Health Organization 2011.
Mulatu.H Magnitude and Factors Associated with Low Birth Weight among New Born in Selected Public Hospitals of Addis Ababa, Ethiopia, 2016 Global Journal of Medical Research: K interdisciplinary Volume 17 Issue 5 Version 1.0 Year 2017
Girma et al. Factors associated with low birthweight among newborns delivered at public health facilities of Nekemte town, West Ethiopia: a case control study BMC Pregnancy and Childbirth (2019) 19:220 https://doi.org/10.1186/s12884-019-2372-x
Asmare et al. Determinants of low birth weight among neonates born in Amhara Regional State Referral Hospitals of Ethiopia: unmatched case control study BMC Res Notes (2018) 11:447 https://doi.org/10.1186/s13104-018-3568-2
Mehare.T Prevalence and Associated Factors of Low Birth Weight among Term Newborns in Dilla Town, Southern Ethiopia International Journal of Pediatrics Volume 2020, Article ID 8394578, 7 pages https://doi.org/10.1155/2020/8394578
Y. Gebregzabiherher, A. Haftu, S. Weldemariam, and H. Gebrehiwet, “The Prevalence and Risk Factors for Low Birth Weight among Term Newborns in Adwa General Hospital, Northern Ethiopia,” Obstetrics and gynecology international, vol. 2017, 7 pages, 2017
Mulatu.H Magnitude and Factors Associated with Low Birth Weight among New Born in Selected Public Hospitals of Addis Ababa, Ethiopia, 2016 Global Journal of Medical Research: K interdisciplinary Volume 17 Issue 5 Version 1.0 Year 2017
Negassi Teklehaimanot, Tesfay Hailu, Huruy Assefa. Prevalence and Factors Associated with Low Birth Weight in Axum and Laelay Maichew Districts, North Ethiopia: A Comparative Cross Sectional Study. International Journal of Nutrition and Food Sciences. Vol. 3, No. 6, 2014, pp. 560-566. doi: 10.11648/j.ijnfs.20140306.21
Alemu. A et al Low birth weight: prevalence and associated factors among newborns at hospitals in Kambata-Tembaro zone, southern Ethiopia 2018 Pan African Medical Journal. 2019; 34:68. doi:10.11604/pamj.2019.34.68.18234
The prevalence of low birth weight and factors associated with low birth weight delivery in Gondar Region, north west Ethiopia Melkie Edris1, Getnet Erakli1
Toru.T et ale Assessment of Low Birth Weight and Associated Factors Among Neonates in Butajira General Hospital, South Ethiopia, Cross Sectional Study, 2019International Journal of Pediatrics Volume 2020, Article ID 5841963, 6 pages https://doi.org/10.1155/2020/5841963
Chanie.H et ale Prevalence of Low Birth Weight and Associated Factors Among Women Delivered in Debre Markos Referral Hospital, East Gojam, Ethiopia, 2017 Journal of Health, Medicine and Nursing Vol.53, 2018
Gebrehawerya, et al., Determinants of Low Birth Weight among Mothers Who Gave Birth in Debremarkos Referral Hospital, Debremarkos Town, East Gojam, Amhara Region, Ethiopia Neonat Pediatr Med 2018, 4:1 DOI: 10.4172/2572-4983.1000145
Mulu.GB et ale Determinants of Low Birth Weight Among Newborns Delivered in Public Hospitals in Addis Ababa, Ethiopia: Case-Control Study Pediatric Health, Medicine and Therapeutics 2020:11 119–126
Dilnessa et al.; Prevalence of Low Birth Weight and Associated Factors among New Born Babies in Ataye Primary Hospital, North Shoa, Ethiopia, 2018 AJMAH, 18(3): 1-11, 2020; Article no. AJMAH.55196
Dadi AF (2015) A Systematic Review and Meta-Analysis of the Effect of Short Birth Interval on Infant Mortality in Ethiopia. PLoS ONE 10(5): e0126759. doi: 10.1371/journal.pone.0126759
Review Manager 5 (RevMan 5) [Computer program]. Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
determinants of low birth weight in neonates born in three hospitals in brong ahafo region adam zakariah this thesis is submitted to the university of ghana, legon in partial fullfilment of the requirements for the award of the master of philosophy degree in applied epidermiology and disease control july 2016
Baur N, Bandyopadhyay G. Socio-Biological Determinants of Low Birth Weight: A Community based study from rural field practice area of Medical College, Kolkata, West Bengal (India) Journal of Dental and Medical Sciences. 2013; 4(4): 33-9
Ismail IM, Venugopalan P. Case-control study on risk factors of low birth weight in a tertiary care hospital, Kerala. Ann Community Health. 2016;4(3):5–12
Matin A et al. Maternal socioeconomic and nutritional determinants of low birth-weight, Shaheed Shohrawardy, medical college hospital, Dhaka, Bangladesh, J Dhaka Med Coll 2008; 17(2) : 83–87
Khanal, V., Zhao, Y., & Sauer, K. (2014). Role of antenatal care and iron supplementation during pregnancy in preventing low birth weight in Nepal: comparison of national surveys 2006 and 2011. Archives of Public Health = Archives Belges de Santé Publique, 72(1), 4. http://doi.org/10.1186/2049-3258-72-4
M. E. Cogswell, I. Parvanta, L. Ickes, R. Yip, and G. M. Brittenham, “Iron supplementation during pregnancy, anemia, and birth weight: a randomized controlled trial,” The American Journal of Clinical Nutrition, vol. 78, no. 4, pp. 773–781, 2003
Ramakrishnan U, González T, Lynnette M, Rivera J, Martorell R. Multiple micronutrient supplementation during pregnancy does not lead to greater infant birth size than does iron-only supplementation: a randomized controlled trial in a semirural community in Mexico. Am J Clin Nutr. 2003; 77(3):720–5
L. H. Allen, “Biological mechanisms that might underlie iron's effects on fetal growth and preterm birth,” The Journal of Nutrition, vol. 131, no. 2, pp. 581S–589S, 2001
Abu-Ouf NM, Jan MM. The impact of maternal iron deficiency and iron deficiency anemia on child’s health. Saudi Med J. 2015;36(2):146
Chaithra A et al. A study on maternal factors affecting low birth weight in institutional deliveries Int J Reprod Contracept Obstet Gynecol. 2020 Oct;9(10):4245-4249