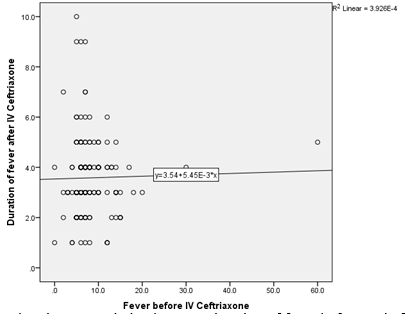
Correlation of duration of IV Ceftriaxone to mean fever clearance time in children with enteric fever
Abstract
Context: Enteric fever is one of the most common and serious infections in a developing country like India. IV ceftriaxone remains the mainstay of therapy in its management. But in a resource-limited setting, the long duration of therapy requiring inpatient admission is not a viable option. The minimum duration of IV ceftriaxone to be given before switching to an oral alternative like cefixime is poorly understood. Fever clearance is one indicator that can be used as a guide for shifting to oral antibiotics. Aims and Objective: To study the minimum duration of IV ceftriaxone before switching to oral cefixime in cases with enteric fever in a resource-limited setting.
Materials and Methods: We performed a cross-sectional study on pediatric patients who were admitted with enteric fever. 170 children admitted to the pediatric ward as enteric fever cases or subsequently diagnosed post fever workup were included in the study. Statistical analysis used: Statistical testing was conducted with the statistical package for the social science system version SPSS 23.0.
Results: Our study showed that only 2.4% of patients had fever beyond one week of ceftriaxone therapy. The mean fever clearance time after initiating IV ceftriaxone was 3.58 days (SD-1.49). No mortality was reported as a complication of enteric fever.
Conclusion: Seven days of IV ceftriaxone followed by seven days of oral cefixime is a reasonable alternative for the treatment of enteric fever in the pediatric population in resource-limited settings.
Downloads
References
John J, Van Aart CJ, Grassly NC. The burden of typhoid and paratyphoid in India: systematic review and meta-analysis. PLoS Negl Trop Dis 2016;10616.
Sinha A, Sazawal S, Kumar R, Sood S, Reddaiah VP, Singh B, et al. Typhoid fever in children aged less than 5 years. The Lancet. 1999 Aug 28;354(9180):734- 7.
Kumar R, Gupta N. Multidrug-resistant typhoid fever. Indian J Pediatr.2007;74:39–42.
Sattar AA, Chowdhury MS, Yusuf MA, Jesmin S, Ara S, Islam MB. Age and Gender Difference of Typhoid Fever among Paediatric Patients Attended at a Tertiary Care Hospital in Bangladesh. Bangladesh J Infect Dis. 2016;3(2):36-9.
Essa F, et al. Study of Socio-Demographic Factors affecting the Prevalence of Typhoid. Ann Med Health Sci Res. 2019;9:469-471.
Garg K N. Mangal, Mathur HC. Clinical profile of multidrug resistant typhoid fever from Jaipur city, Indian Pediatr. 1994 Feb;31:191-192.
Arora RK, Gupta A, Joshi NM, Kataria VK, Lall P, Anand AC.Multidrug resistant typhoid fever study of an outbreak in Calcutta. Indian Pediatr.1992;29:62-63.
Jeeyani HN, Prajapati BS, Bloch A. Enteric Fever in Children-Clinical profile, sensitivity patterns and response to antimicrobials. GCSMC J Med Sci. 2015;4(1):40-3.
Sharma P, Dahiya S, Manral N, Kumari B, Kumar S, Pandey S, et al. Changing trends of culture-positive typhoid fever and antimicrobial susceptibility in a tertiary care North Indian Hospital over the last decade. Indian J Med Microbiol. 2018 Jan 1;36(1):70.
Das JC. Laboratory investigations of enteric fever in children: an update.JCMCTA. 2007; 18(2):37-42.
Chowta MN, Chowta NK. Study of clinical profile and antibioticresponse in typhoid fever. Indian J Med Microbiol.2005; 23:125-127.
Thompson CN, Karkey A, Dongol S, Arjyal A, Wolbers M, et al. Treatment response in enteric fever in an era of increasing antimicrobial resistance: an individual patient data analysis of 2092 participants enrolled into 4 randomized, controlled trials in Nepal. Clin Infect Dis. 2017;64:1522–1531.