Study of clinical profile and surgical outcome of pterygium in adult patients at rural tertiary care hospital.
Abstract
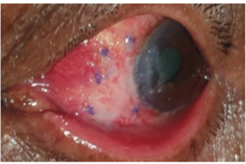
Introduction: Pterygium is a benign, degenerative condition of the subconjunctival tissue, for which many surgical techniques ranging from McReynaud’s operation to conjunctival autograft and amniotic membrane graft, have been discussed in the literature. Grafts prevent a recurrence, acting as a barrier, and have proven to be the gold standard. Here we have studied the clinical profile and surgical outcome of pterygium surgery by various techniques at a Rural tertiary care hospital (RTCH).
Aims/ Objectives: Our primary aim was to study demographical factors and clinical profile of pterygia along with the surgical outcome and postoperative complications of pterygium surgery by various techniques, at RTCH.
Materials and Methods: In this, hospital-based observational descriptive longitudinal study, we studied 75 patients, with primary progressive pterygium, who underwent pterygium surgery from September 2019- March 2021 and recorded their pre-operative, intraoperative, and postoperative data with a follow-up period of 3 months. Results: 74.6% of the population were females, with a bimodal peak incidence in 31-40 years and 61-70 years (22.6%). Most common presentation in both eyes (46.6%) with 97.3% cases presenting with nasal pterygium. 66.6% of patients presented with a grade 2 pterygium. 50 patients had a pre-operative “with the rule astigmatism”. Pre-operative keratometry readings could not be assessed for 5 patients due to excessive distortion of the corneal surface. 37 patients underwent graft fixation with no suture no glue while 38 patients underwent graft fixation with sutures. The most common complication was graft edema which was seen in 53 patients, while recurrence was seen in 2 patients.
Conclusion: The occurrence of pterygium is very common in rural areas, which in most cases, is neglected due to lack of awareness. Surgical excision with conjunctival autograft continues to be the gold standard of treatment for the same.
Downloads
References
Sarkar P, Tripathy K. Pterygium. [Updated 2021 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558907/
Weinstein, O., Rosenthal, G., Zirkin, H., et al. Overexpression of p53 tumor suppressor gene in pterygia. Eye 16, 619–621 (2002). https://doi.org/10.1038/sj.eye.6700150
http://ocularcentre.com/wp-content/uploads/2015/01/Surgical-Management-of-Pterygium.pdf
Das S, Ramamurthy B, Sangwan VS. Deep lamellar keratoplasty for recurrent advanced pterygium. Ophthalmic Surg Lasers Imaging. 2009 Jan-Feb;40(1):43-5. doi: 10.3928/15428877-20090101-06. PMID: 19205495.
Das AV, Podila S, Prashanthi GS, Basu S. Clinical profile of pterygium in patients seeking eye care in India: electronic medical records-driven big data analytics report III. Int Ophthalmol. 2020 Jun;40(6):1553-1563. doi: 10.1007/s10792-020-01326-3. Epub 2020 Feb 24. PMID: 32096104.
Hashemi, Hassan et al. “The prevalence and determinants of pterygium in rural areas.” Journal of current ophthalmology vol. 29,3 194-198. 11 Nov. 2016, doi:10.1016/j.joco.2016.09.002
Nemesure B, Wu SY, Hennis A, Leske MC; Barbados Eye Studies Group. Nine-year incidence and risk factors for pterygium in the barbados eye studies. Ophthalmology. 2008 Dec;115(12):2153-8. doi: 10.1016/j.ophtha.2008.08.003. Epub 2008 Oct 18. PMID: 18930552.
Cajucom-Uy H, Tong L, Wong TY, Tay WT, Saw SM. The prevalence of and risk factors for pterygium in an urban Malay population: the Singapore Malay Eye Study (SiMES). Br J Ophthalmol. 2010 Aug;94(8):977-81. doi: 10.1136/bjo.2008.150847. Epub 2009 Dec 3. PMID: 19965830.
Dasgupta, Sushobhan. (2016). Pterygium excision with suture-free, glue-free conjunctival autograft (SFGF-CAG): Experience of a tertiary care hospital of Northern India. Journal of Clinical Ophthalmology and Research. 4. 143-48. 10.4103/2320-3897.190788
Avisar R, Loya N, Yassur Y, Weinberger D. Pterygium-induced corneal astigmatism. Isr Med Assoc J. 2000 Jan;2(1):14-5. PMID: 10892364.
Salagar, Kavita Mallikarjun, and Kalyanappa Gurlingappa Biradar. “Conjunctival autograft in primary and recurrent pterygium: a study.” Journal of clinical and diagnostic research: JCDR vol. 7,12 (2013): 2825-7. doi:10.7860/JCDR/2013/7383.3767