Axillary lymph node status according to location, size, number and grading among breast cancer patients in tertiary care hospitals, Bangladesh
Abstract
Background: There are a good number of tumor-related features available to predict the prognosis of breast cancer and its stage of severity. Axillary lymph node status according to the location, size, number, and grading among breast cancer patients have a potential prognostic value in the course of breast cancer treatment, mortality, and morbidity. We have very limited researched-based information regarding these issues.
Aim of the study: The aim of this study was to assess the axillary LN status according to location and grade of tumor also size and number of axillary LN among breast cancer patients.
Methods: This was axillary LN status according to the location of a prospective observational study conducted in the Department of Surgery & Oncology, Dhaka Medical College Hospital, BSMMU, and NICRH Dhaka, Bangladesh during the period from January 2015 to December 2016. In total 100 patients of several age groups with breast cancer, patients attended, diagnosed, and treated in the mentioned hospital were selected as the study subjects. Proper clinical examination and ultrasonography for the assessment of axillary lymph node status were done for every participant. All data were processed, analyzed, and disseminated by MS Office and SPSS program as per need.
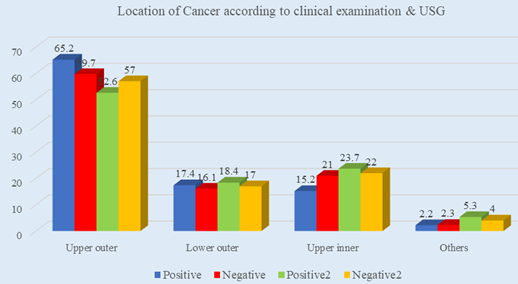
Results: In location analysis, we observed, most of the tumors were located in the upper outer quadrant (57%) followed by 22.0%, 17.0%, and 4.0% were located in the upper inner quadrant, lower outer quadrant, and in other locations respectively. Most of the tumors were of Grade II (67%) followed by 21.0% and 12.0% were of grade I and grade III respectively. Maximum 52.5% patients of this study had a lymph node with the size of 1-2 cm followed by 25.0% and 22.5% patients had lymph nodes with the size of >2cm and 9. Both clinical examination and USG showed positive results in increasing the number of lymph nodes.
Conclusion: In analyzing the location, size, number, and grading of axillary lymph node among breast cancer patients by using clinical examination and USG findings, we found statistically significant correlations in the size and number of the lymph node. So, we can conclude that the location & grade of tumor and number & size of axillary lymph node among breast cancer patients are the most potent indicators of severity and status of breast cancer.
Downloads
References
Chakraborty, A., Bose, C. K., Basak, J., Sen, A. N., Mishra, R., & Mukhopadhyay, A. (2016). Determinants of lymph node status in women with breast cancer: A hospital-based study from eastern India. The Indian journal of medical research, 143(Suppl 1), S45.
Jatoi I, Hilsenbeck SG, Clark GM, Osborne CK. Significance of axillary lymph node metastasis in primary breast cancer. J Clin Oncol 1999; 17: 2334-40.
Warren LE, Punglia RS, Wong JS, et al. Management of the regional lymph nodes following breast-conservation therapy for early-stage breast cancer: an evolving paradigm. Int J Radiat Oncol Biol Phys 2014; 90:772–7.
Williams PA, Suggs J, Mangana SH. Axillary lymph node treatment in breast cancer: an update. J Miss State Med Assoc 2014; 55:145–7.
Hernandez-Aya LF, Chavez-Macgregor M, Lei X, et al. Nodal status and clinical outcomes in a large cohort of patients with triple-negative breast cancer. J Clin Oncol 2011; 29:2628–34.
Wang CW, Kuo WH, Chang KJ, et al. should adjuvant radiotherapy to the supraclavicular fossa be routinely given in patients with breast conservative treatment? J Surg Oncol 2007; 96:144–50.
Valente SA, Levine GM, Silverstein MJ, et al. Accuracy of predicting axillary lymph node positivity by physical examination, mammography, ultrasonography, and magnetic resonance imaging. Ann Surg Oncol 2012; 19:1825–30.
Neal CH, Daly CP, Nees AV, et al. Can preoperative axillary US help exclude N2 and N3 metastatic breast cancer? Radiology 2010; 257: 335–41.
Tate J J T, Lewis V, Archer T, Guyer P G, Royale G T, Taylor I. Ultrasound detection of axillary lymph node metastases in breast cancer. Eur J Surg Oncol 1989; 15: 139–141.
Deurloo EE, Tanis PJ, Gilhuijs KG, Muller SH, Kroger R, Peterse JL, Rutgers EJ, Valdes Olmos R, Schultze Kool LJ. Reduction in the number of sentinel lymph node procedures by preoperative ultraso- nography of the axilla in breast cancer. Eur J Cancer 2003; 39: 1068–1073.
Rajesh YS, Ellenbogen1 IS Banerjee B. Preoperative axillary ultrasound scan: its accuracy in assessing the axillary nodal status in carcinoma breast doi:10.1054/brst.2001.0352. The Breast (2002) 11, 49–52.
Halsted W S. The results of operations for the cure of cancer of the breast performed at The Johns Hopkins Hospital from June 1889 to January 1894. Johns Hopkins Hospital Rep. 4 1894; 297–350.
García Fernández A, Fraile M, Giménez N, et al. Use of axillary ultrasound, ultrasound-fine needle aspiration biopsy and magnetic resonance imaging in the preoperative triage of breast cancer patients considered for sentinel node biopsy. Ultrasound Med Biol 2011; 37: 16–22.
Park SH, Kim MJ, Park BW, et al. Impact of preoperative ultrasonography and fine-needle aspiration of axillary lymph nodes on surgical management of primary breast cancer. Ann Surg Oncol 2011; 18: 738–44.
Chen, W., Wang, C., Fu, F., Yang, B., Chen, C., & Sun, Y. (2020). A model to predict the risk of lymph node metastasis in breast cancer based on clinicopathological characteristics. Cancer Management and Research, 12, 10439.
Zhang, Y., Li, J., Fan, Y., Li, X., Qiu, J., Zhu, M., & Li, H. (2019). Risk factors for axillary lymph node metastases in clinical stage T1-2N0M0 breast cancer patients. Medicine, 98(40).