Study of intraoperative challenges and early surgical outcome of phacoemulsification through temporal incision in patients with senile cataract at rural tertiary care hospital.
Abstract
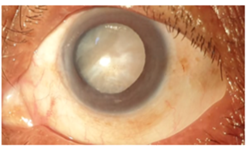
Introduction: Temporal phacoemulsification (Phaco) gives a better surgical outcome in senile cataracts as it nullifies, “against the rule astigmatism” which is common in elderly patients. It is a well-established, effective and safe technique. We conducted this study to verify the surgical outcome of temporal phacoemulsification at a rural tertiary care hospital (RTCH).
Aims and Objectives: To study the intra operative and early post-operative complications, post-operative UCVA (Uncorrected Visual Acuity) and BCVA (Best Corrected Visual Acuity) in patients with senile cataract who underwent temporal phacoemulsification.
Materials and Methods: In this prospective, hospital-based observational study, we studied intraoperative and postoperative data of 42 patients, above 50 years of age, who underwent temporal phacoemulsification for senile cataracts from August 2019 to May 2020 after obtaining institutional ethical committee approval and written informed consent from all patients. All patients underwent minimum 6 weeks of postoperative follow-up.
Results: Out of 42 patients, 57.14% were females and the most common age group was 61-70 years. Intraoperative bleeding was seen in 19.04% of patients and the post-operative mild corneal stromal haze and mild uveitis were seen in 4.76% and 7.14% of patients on a postoperative day 1(POD 1) respectively. Reduction in preoperative “against the rule astigmatism” was seen in 68% of patients. All patients had a UCVA of >6/12 and a BCVA of 6/6 at the last follow-up.
Conclusion: Temporal phacoemulsification gives a good UCVA and faster visual rehabilitation in patients with senile cataracts.
Downloads
References
Nirmalan PK, Robin AL, Katz J. Risk factors for age-related cataract in a rural population of southern India: The Aravind Comprehensive Eye Study. British Journal of Ophthalmology 2004; 88:989-994.
Raina, B., & Sharma, P. (2020). The study of the demographic profile of patients of senile mature cataract attending the eye OPD of GMC Jammu, India. International Journal of Research in Medical Sciences, 8(3), 833-835. doi:http://dx.doi.org/10.18203/2320-6012.ijrms20200481
Malik VK, Kumar S, Kamboj R, et al. Comparison of astigmatism following manual small incision cataract surgery-superior and temporal approach. Nepal J Ophthalmol 2012; 4; 7:54-58.
Al Mahmood AM, Al-Swailem SA, Behrens A. Clear corneal incision in cataract surgery. Middle East Afr J Ophthalmol. 2014 Jan-Mar;21(1):25-31. doi: 10.4103/0974-9233.124084. PMID: 24669142; PMCID: PMC3959037
Fine IH. Clear corneal incisions. Int Ophthalmol Clin. 1994;34(2):59-72. doi:10.1097/00004397-199403420-00005
Grzybowski, A., Kanclerz, P. Do we need day-1 postoperative follow-up after cataract surgery? Graefes Arch Clin Exp Ophthalmol 257, 855–861 (2019).
Abrar Ali, Tabassum Ahmed, Tahir Ahmed. Corneal problems during and after phacoemulsification by beginner phacoemulsification surgeon. Pak J Med Sci May - June 2007 Vol. 23 No. 3 401-404.
Findl O, Amon M, Petternel V, Kruger A. Early objective assessment of intraocular inflammation after phacoemulsification cataract surgery. J Cataract Refract Surg. 2003 Nov;29(11):2143-7. doi: 10.1016/s0886-3350(03)00411-5. PMID: 14670423.
Nikose AS, Saha D, Laddha PM, Patil M. Surgically induced astigmatism after phacoemulsification by temporal clear corneal and superior clear corneal approach: a comparison. Clin Ophthalmol. 2018 Jan 3; 12:65-70. doi: 10.2147/OPTH.S149709. PMID: 29379266; PMCID: PMC5757199.
Roman S, Ullern M. Astigmatisme induit par les incisions cornéennes supérieures et temporales dans la chirurgie de la cataracte [Astigmatism caused by superior and temporal corneal incisions in cataract surgery]. J Fr Ophtalmol. 1997;20(4):277-83. French. PMID: 9181139
Snehal P Gade, Bhaskar S Khaire.The visual outcome with superior, superotemporal and temporal incisions used in phacoemulsification surgery - a comparative study. MedPulse – International Medical Journal, ISSN: 2348-2516, EISSN: 2348-1897, Volume 1, Issue 8, August 2014 pp 429-433
Holladay JT, Cravy TV, Koch DD. Calculating the surgically induced refractive change following ocular surgery. J Cataract Refract Surg 1992; 18:429‐43.
Kohnen T, Dick B, Jacobi KW. Comparison of the induced astigmatism after temporal clear corneal tunnel incisions of different sizes. J Cataract Refract Surg 1995; 21:417‐24.