Unrecognized renal dysfunction in patients with acute stroke- Cross sectional study
Abstract
Background and Objectives: Unrecognized renal insufficiency, defined as an estimated glomerular filtration rate <60 mL/min/l .73 m2 in the presence of normal serum creatinine levels, is a common comorbid condition among patients with various cardiovascular conditions. The current study was aimed to evaluate the prevalence and clinical significance of unrecognized renal dysfunction in patients admitted with acute stroke.
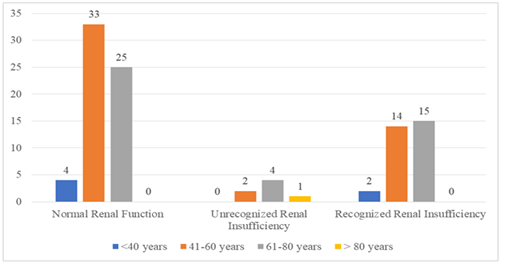
Patients & Methods: This cross sectional study consisted of patients with acute stroke admitted in medical ward at Stanley medical college. Estimated glomerular filtration is estimated using MDRD and CKD — EPI formula. Study group is divided into three groups (Normal renal function, Unrecognized and Recognized renal dysfunction) as per eGFR. The two primary outcomes such as severe disability at hospital discharge and in-hospital mortality are compared in each group.
Results: Of the 100 patients with stroke included in the study, 62% had a normal renal function, 31% had recognized renal insufficiency, and 7% had unrecognized renal insufficiency. Mortality rates are higher in patients with recognized and unrecognized renal insufficiency compared with patients with normal renal function (29% and 28.5% and 9.6%) respectively, P <0.04053). Similarly, severe disability rates at discharge are also higher in patients with recognized and unrecognized renal insufficiency compared with patients with normal renal function (72.27%, 80 %, and 32.14%) respectively.
Conclusion: Unrecognized renal insufficiency is common among patients with acute stroke and is associated with adverse short-term outcomes.
Downloads
References
Pereg, D., Rozenbaum, Z., Vorobeichik, D., Shlomo, N., Gilad, R., Bloch, S., Mosseri, M. and Tanne, D., 2016. Prevalence and Significance of Unrecognized Renal Dysfunction in Patients with Stroke. The American journal of medicine, 129(10), pp. 1074-1081.
Florkowski, c.M. and Chew-Harris, J.s., 2011. Methods of estimating GFRdifferent equations including CKD-EPI. The Clinical Biochemist Reviews, 32(2),p.75.
Inker, L.A. and Levey, AS., 2013. Pro: Estimating GFR using the chronic kidney disease epidemiology collaboration (CKD-EPI) 2009 creatinine equation: the time for change is now, Nephrologv Dialysis Transplantation, 28(6), pp. 1390-1396.
Snarska, K., Kapica-Topczewska, K., Bach6rzewska-Gajewska, H. and Malyszko, J., 2016. Renal Function Predicts Outcomes in Patients with Ischaemic Stroke and Haemorrhagic Stroke. Kidney and Blood Pressure Research, 41(4), pp.424-433.
Mac Walter, R.s., Wong, s.Y., Wong, K.Y., Stewart, G., Fraser, c.G., Fraser, H. W. , Ersoy, Y., Ogston, S.A. and Chen, R., 2002. Does renal dysfunction predict mortality after acute stroke?. Stroke, 33(6), pp. 1630-1635.
Tsagalis, G., Akrivos, T., Alevizaki, M., Manios, E., Stamatellopoulos, K. , Laggouranis, A. and Vemmos, K.N., 2008. Renal dysfunction in acute stroke: an independent predictor of long-term all combined vascular events and overall mortality. Nephrology Dialysis Transplantation, I ), pp. 194-200.
Easton, J.D., Saver, J.L., Albers, G.W., Alberts, M.J., Chaturvedi, S., Feldmann, E., Hatsukami, T.S., Higashida, R.T., Johnston, S.C., Kidwell, C.S. and Lutsep, H.L., 2009. Definition and evaluation of transient ischemic attack. Stroke, 40(6), pp.2276-2293.
Prowle, J.R., Ishikawa, K., May, C.N. and Bellomo, R., 2010. Renal plasma flow and glomerular filtration rate duringacute kidney injury in man. Renal failure, 32(3), pp.349-355.
Fisher, M. and Furie, K., 2017. Practicing Evidence-Based Stroke Medicine
Zacharia, B.E., Ducruet, A.F., Hickman, Z.L., Grobelny, B.T., Fernandez, L., Schmidt, J.M., Narula, R., Ko, L.N., Cohen, M.E., Mayer, S.A. and Connolly, E.S., 2009. Renal dysfunction as an independent predictor of outcome after aneurysmal subarachnoid hemorrhage. Stroke, 40(7), pp.2375-2381.
Neaton JD, Wentworth DN, Cutler J, Stamier J, Kuller L. Risk factors for death from different types of stroke. Multiple Risk Factor Intervention Trial. Research Group. Ann Epidemiol. 1993:3 :393 493-499
Arboix, A., 2015. Cardiovascular risk factors for acute stroke: Risk profiles in the different subtypes of ischemic stroke. World Journal of Clinical Cases: WJCC, 3(5), p.418.
Sandilands, E.A., Dhaun, N., Dear, J.W. and Webb, D.J., 2013. Measurement of renal function in patients with chronic kidney disease. British journal of clinical pharmacologv, 76(4), pp.504-515.
Anupama, Y.J. and Uma, G., 2014. Prevalence of chronic kidney disease among adults in a rural community in South India: Results from the kidney disease screening (KIDS) project. Indian journal of nephrology, 24(4), P•214 '
Eswarappa, M., Gireesh, M.S., Ravi, V., Kumar, D. and Dev, G., 2014. The spectrum of acute kidney injury in critically ill patients: A single-center study from South India. Indian journal of nephrology, 24(5), p.280.
Reddy, N.P.K., Annigeri, R., Ramakrishnan, N. and Venkataraman, R., 2014. Epidemiology, outcomes, and validation of RIFLE and AKIN criteria in acute kidney injury (AKI) in critically ill patients: Indian perspective. Renal failure, 36(6), pp.831-837.
Kumar, S., Selim, M.H. and Caplan, L.R., 2010. Medical complications after stroke. The Lancet Neurology, 9(l), pp. 105-118.
Eddy, A.A., 2005. Progression in chronic kidney disease. Advances in chronic kidney disease, 12(4), pp.353-365.