A study of the prognostic value of red cell distribution width and neutrophil: lymphocyte ratio in adults with sepsis
Abstract
Introduction: Sepsis continues to be a major cause of morbidity and mortality in Intensive Care Units (ICU) despite the better understanding of its pathophysiology in recent years. This may manifest as organ dysfunction such as hypotension, altered mental status, abnormal coagulation, increase in bilirubin levels, deranged renal function and increase in oxygen requirements. With this background, the current study of the relationship between RDW and neutrophil: lymphocyte ratio with severity of illness in patients admitted to medical ICUs with sepsis, has been undertaken.
Objectives: To study the prognostic value of red cell distribution width and neutrophil: lymphocyte ratio in sepsis.
Materials and Methods: This study was conducted on adult patients, who were admitted in ICUs of Tertiary care hospitals attached to Dr. VVP RMC, Loni, Maharashtra and whose haematological investigations were done within 24 hours of ICU admission. Patients with haematological disorders, immunocompromised patients, patients whose haematological investigations were not done within 24 hours of admission and who were not admitted in ICU were excluded from the study. The study was conducted for a two-year timespan, from September 2020 to September 2022. On admission, patients were stratified according to q-SOFA scoring10 and SOFA score were calculated. Haematological investigations were done within 24 hours of admission. q-SOFA score and SOFA score were calculated at the fifth day of admission to ICU, to assess progress of the patient.
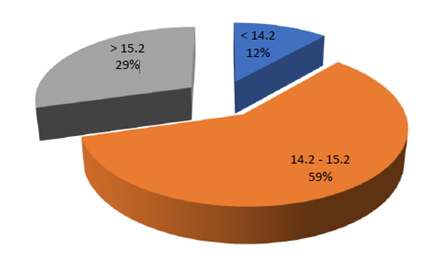
Results: Majority of the patients with sepsis were over 50 years of age. Hypertension, diabetes and obstructive airway diseases were the most common comorbidities present in the patients that were present in the study. Pulmonary infections were the most common source of infection in majority of sepsis cases, followed by tropical/ non- localised infections. RDW was found to be between 14.2 and 15.2 in majority of patients with sepsis in the study group. It was found that higher the RDW, higher the q-SOFA score and worse is the outcome at the end of 5 days. RDW at admission vs Outcomes assessed using ANOVA obtained a p value of p<0.0001 (highly significant). Patients with worse outcomes had a high RDW at admission. NLR vs q-SOFA assessed using Kruskal Wallis and then checked using Mann Whitney U test showed a significant p value of 0.006. It was found in the study that as the q-SOFA score increases, median NLR increases.
Conclusion: The study implies that patients with sepsis having an RDW more than 15.050 may benefit from early interventions and more aggressive management. In low resource settings, the RDW, in the emergency department could afford the earliest opportunity to identify patients at risk of bacteremia and the administration of antimicrobials at the appropriate time.
Downloads
References
Martin GS. Sepsis, severe sepsis and septic shock: changes in incidence, pathogens and outcomes. Expert review of anti-infective therapy. 2012 Jun 1;10(6):701-6.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS. The third international consensus definitions for sepsis and septic shock (Sepsis-3). Jama. 2016 Feb 23;315(8):801-10.
Stearns-Kurosawa DJ, Osuchowski MF, Valentine C, Kurosawa S, Remick DG. The pathogenesis of sepsis. Annual review of pathology: mechanisms of disease. 2011 Feb 28;6:19-48.
Mahmood NA, Mathew J, Kang B, DeBari VA, Khan MA. Broadening of the red blood cell distribution width is associated with increased severity of illness in patients with sepsis. International journal of critical illness and injury science. 2014 Oct;4(4):278.
Zahorec R. Ratio of neutrophil to lymphocyte counts-rapid and simple parameter of systemic inflammation and stress in critically ill. Bratislavske lekarske listy. 2001 Feb;102(1):5-14.
Salciccioli JD, Marshall DC, Pimentel MA, Santos MD, Pollard T, Celi LA, Shalhoub J. The association between the neutrophil-to-lymphocyte ratio and mortality in critical illness: an observational cohort study. Critical Care. 2015 Dec;19(1):13.
Akilli NB, Yortanlı M, Mutlu H, Günaydın YK, Koylu R, Akca HS, Akinci E, Dundar ZD, Cander B. Prognostic importance of neutrophil-lymphocyte ratio in critically ill patients: short-and long-term outcomes. The American journal of emergency medicine. 2014 Dec 1;32(12):1476-80.
de Jager CP, van Wijk PT, Mathoera RB, de Jongh-Leuvenink J, van der Poll T, Wever PC. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Critical care. 2010 Oct;14(5):R192.
Shaikh MA, Yadavalli DR. Red cell distribution width as a prognostic marker in severe sepsis and septic shock. International Journal of Advances in Medicine. 2017 May;4(3):750.
Kaukonen KM, Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic inflammatory response syndrome criteria in defining severe sepsis. New England Journal of Medicine. 2015 Apr 23;372(17):1629-38.
Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, Angus DC, Reinhart K. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. American journal of respiratory and critical care medicine. 2016 Feb 1;193(3):259-72.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G. 2001 sccm/esicm/accp/ats/sis international sepsis definitions conference. Intensive care medicine. 2003 Apr 1;29(4):530-8.
Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis. Critical care medicine. 2006 Jan 1;34(1):15-21.
Deen J, Von Seidlein L, Andersen F, Elle N, White NJ, Lubell Y. Community-acquired bacterial bloodstream infections in developing countries in south and southeast Asia: a systematic review. The Lancet infectious diseases. 2012 Jun 1;12(6):480-7.
Chandrasekar PH, Brown WJ. Clinical issues of blood cultures. Archives of internal medicine. 1994 Apr 25;154(8):841-9.
Angele MK, Pratschke S, Hubbard WJ, Chaudry IH. Gender differences in sepsis: cardiovascular and immunological aspects. Virulence. 2014 Jan 1;5(1):12-9.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992 Jun 1;101(6):1644-55.
Rhee C, Jones TM, Hamad Y, Pande A, Varon J, O’Brien C, Anderson DJ, Warren DK, Dantes RB, Epstein L, Klompas M. Prevalence, underlying causes, and preventability of sepsis-associated mortality in US acute care hospitals. JAMA network open. 2019 Feb 1;2(2):e187571-.
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D. Sepsis in European intensive care units: results of the SOAP study. Critical care medicine. 2006 Feb 1;34(2):344-53.
Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, Schorr C, Artigas A, Ramsay G, Beale R, Parker MM. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive care medicine. 2010 Feb 1;36(2):222-31.
Gander RM, Byrd L, DeCrescenzo M, Hirany S, Bowen M, Baughman J. Impact of blood cultures drawn by phlebotomy on contamination rates and health care costs in a hospital emergency department. Journal of clinical microbiology. 2009 Apr 1;47(4):1021-4.
Dorsher CW, Rosenblatt JE, Wilson WR, Ilstrup DM. Anaerobic bacteremia: decreasing rate over a 15-year period. Reviews of infectious diseases. 1991 Jul 1;13(4):633-6.
Schmidt M, Mandel J, Sexton DJ, Hockberger RS. Evaluation and management of suspected sepsis and septic shock in adults. Up-to-date. Available online: https://www. up-to-date. com/contents/evaluation-and-management-of-suspected-sepsisand-septic-shock-in-adults (accessed on 29 September 2017). 2016 Dec.
Hwang SY, Shin TG, Jo IJ, Jeon K, Suh GY, Lee TR, Yoon H, Cha WC, Sim MS. Neutrophil-to-lymphocyte ratio as a prognostic marker in critically-ill septic patients. The American journal of emergency medicine. 2017 Feb 1;35(2):234-9.
Churpek MM, Zadravecz FJ, Winslow C, Howell MD, Edelson DP. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. American journal of respiratory and critical care medicine. 2015 Oct 15;192(8):958-64.