Effect of glycaemic status in neonatal sepsis-A prospective observational study
Abstract
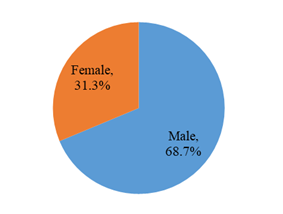
Introduction: Neonatal hypoglycemia is a common and readily treatable risk factor for neurologic impairment in children. Although associations between prolonged symptomatic neonatal hypoglycemia and brain injury are well established, the effect of milder hypoglycemia on neurologic development is uncertain. Objective: To determine the glycemic status among patients with neonatal sepsis and to evaluate their association with the mortality. Methods: It was a prospective observational study conducted at Department of Pediatrics, Rajshahi Medical College Hospital, Rajshahi, Bangladesh from July 2021 to June 2022. Total 52 patients clinically diagnosed as neonatal sepsis were studied, a detailed history and thorough physical examination was done in each patient on admission. History included age of newborn, sex, gestational age, h/o prolonged rupture of membrane (PROM), intrapartum fever or fever 3 days before delivery, per vaginal foul smelling discharge, prolonged labor and features of sepsis. Physical examination included respiratory rate, heart rate, temperature, chest indrawing, grunting, cyanosis, convulsion, breath sound, added sound, weight, jaundice, bleeding manifestation, status of fontanelles, umbilicus and capillary refill time. Blood glucose level and mortality of neonates having hypoglycemia and hyperglycemia were analyzed. Results: Out of 52 patients clinically diagnosed as neonatal sepsis were studied. The mean age was found 10.2±8.4 days with range from 1 to 28 days and more than half (51.6%) patients belonged to age ≤7 days. More than two third (68.7%) patients were male and 31.3% were female. 42(80.77%) patients were found CRP positive and 10(19.23%) were negative CRP. 34.62% patients were blood culture positive and 65.38% patients were culture negative. Majority (71.43%) of CRP positive patients were found normoglycemic, 11.90% were found hypoglycemic and only 16.67% were found hyperglycemic. Among 18 culture positive patients 11(61.11%) were normoglycaemic, 3(16.67%) were hypoglycemic and 4(22.22%) were hyperglycemic. 57.1% of hyperglycemic and 40% of hypoglycemic patients were died whereas only 13.3% of normoglycemic patients were died. Out of 10 expired patients, 2 patients Hypoglycemia, 4 patients Normoglycemia and 4 patients Hyperglycemia. Mortality was high in Hypoglycemia patient (40.0%) in comparison with normoglycaemic patient (13.33%) and the difference was not statistically significant (p>0.05) between two groups. Mortality was also high in hyperglycaemic patient (57.14%) in comparison with normoglycaemic patient (13.33%) and the difference was statistically significant (p<0.05) between two groups. Conclusion: Alteration of glycemic status occurred in septic newborn. Our study showed mortality is higher among the septic newborn with hyperglycemia. The incidence of hypoglycemia was high as compared to hyperglycemia. Neonatal hypoglycemia and hyperglycemia was a significant factor in the overall mortality in neonatal sepsis.
Downloads
References
Boluyt N, van Kempen A, Offringa M. Neurodevelopment after neonatal hypoglycemia: a systematic review and design of an optimal future study. Pediatrics. 2006; 117:2231–43.
Adamkin DH. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2011; 127:575–9.
Harris DL, Weston PJ, Harding JE. Incidence of neonatal hypoglycemia in babies identified as at risk. J Pediatr. 2012; 161:787–91.
March of Dimes Perinatal Data Center. Special care nursery admissions. 2011 http://www.marchofdimes.org/peristats/pdfdocs/nicu_summary_final.pdf.
Wilker RE. Hypoglycemia and Hyperglycemia. In: Cloherty JP, Eichenwald EC, Stark AR, editors. Manual of Neonatal Care. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2008. p. 540-49.
Harris DL, Weston PJ, Signal M, Chase JG, Harding JE. Dextrose gel for neonatal hypoglycaemia (the Sugar Babies Study): a randomised, double-blind, placebo-controlled trial. Lancet. 2013; 382:2077–83.
Ranger M, Chau CM, Garg A, et al. Neonatal pain-related stress predicts cortical thickness at age 7 years in children born very preterm. PLoS One. 2013;8(10):e76702.
Hay WW, Jr, Raju TN, Higgins RD, Kalhan SC, Devaskar SU. Knowledge gaps and research needs for understanding and treating neonatal hypoglycemia: workshop report from Eunice Kennedy Shriver National Institute of Child Health and Human Development. J Pediatr. 2009; 155:612–7.
Harris DL, Weston PJ, Williams CE, et al. Cot-side electroencephalography monitoring is not clinically useful in the detection of mild neonatal hypoglycemia. J Pediatr. 2011; 159:755–60.
Ahmad S, Khalid R. Blood Glucose Levels in Neonatal Sepsis and Probable Sepsis and its Association with Mortality. Journal of the College of Physicians and Surgeons Pakistan. 2012; 22: 15-18.
Begum S, Baki MA, Kundu GK, Islam I, Kumar M, Haque A. Bacteriological Profile of Neonatal Sepsis in a Tertiary Hospital in Bangladesh. J Bangladesh Coll Phys Surg. 2012; 30: 66-70.
Wintergerst KA, Buckingham B, Gandrud L, Wong BJ, Kache S, Wilson DM. Association of hypoglycemia, hyperglycemia, and glucose variability with morbidity and death in pediatric intensive care unit. Pediatrics. 2006; 118:173-79.