Role of Serum Lactate Dehydrogenase (LDH) and endometrial thickness in the detection of endometrial carcinoma in perimenopausal bleeding
Abstract
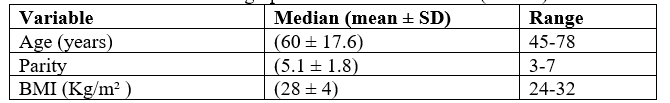
Introduction: Postmenopausal bleeding (PMB) refers to any uterine bleeding in a menopausal patient (other than the expected cyclic bleeding that occurs in patients taking combined (ie, estrogen-progestin), cyclic, postmenopausal hormone therapy. Perimenopausal bleeding (PMB) occurs in approximately 3% of women and it is the usual presenting symptom of endometrial carcinoma in approximately 93% of cases. Objective: To assess the role of serum lactate dehydrogenase (LDH) and endometrial thickness in the detection of endometrial carcinoma in perimenopausal bleeding. Methods: This prospective cross-sectional study was carried out at Obstetrics and Gynecology Department, Rajshahi Medical College Hospital, Rajshahi, Bangladesh from January 2020 to June 2022. This study included 102 women with perimenopausal bleeding admitted to Obstetrics & Gynecology Department at RMCH. All cases were subjected to full history, full clinical examination, transvaginal sonography, serum LDH, and Diagnostic endometrial biopsy was taken for histopathological examination. Result: In this study, endometrial thickness at 11.5mm cut-off value showed 80.6% sensitivity, 53.7% specificity, PPV 53.7%, NPV 80.5%and diagnostic accuracy 64.4%. It was found that TVS evaluation of endometrial thickness is not sensitive enough to detect cancer of the endometrium and therefore, could not replace the histological evaluation of the endometrial tissue in women with postmenopausal bleeding. LDH level cutoff value of 430 U/L could differentiate malignant from benign lesions with a sensitivity of 80.6%, specificity of 57.4%, PPV of 55.7% and NPV of 81.5% with a diagnostic accuracy of 66.7%. Thus, total serum LDH can be used as a good negative test using the cut-off level (430 U/L). A combination of evaluation of endometrial thickness by TVS (with a specificity of 53.7% and accuracy of 64.4%) and serum LDH (with a specificity of 57.4% and accuracy of 66.7%) increase the specificity to 72.2%. also, increase the accuracy to 67.7%. Conclusion: Measurement of serum LDH is considered another simple method to be combined with TVS if endometrial cancer is suspected. However, further studies are needed using LDH isoenzymes profile and TVS endometrial morphology.
Downloads
References
Mansour GM, El-Lamie IK, El-Kady MA, El-Mekkawi SF, Laban M, Abou-Gabal AI. et al. Endometrial volume as predictor of malignancy in women with postmenopausal bleeding. Int J Gynaecol Obstet. 2007; 99:206-10.
Timmermans MB, Gerritse BC, Opmeer FW, Jansen BW Mol, Veersema S. “Diagnostic accuracy of endometrial thickness to exclude polyps in women with postmenopausal bleeding,” Journal of Clinical Ultrasound. 2008; 36(5):286- 290.
Baser E, Gungor T, Togrul C, Turkoglu O, Celen S. Preoperative prediction of poor prognostic parameters and adjuvant treatment in women with pure endometrioid type endometrial cancer: what is the significance of tumor markers? Eur J Gynaecol Oncol. 2014; 35(5):513-8
Creasman WT, Odicino F, Maisonneuve P, et al. Carcinoma of the corpus uteri: FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006;95(suppl 1): S105-S143. doi:10.1016/S0020-7292(06)60031-3
UK CR. Uterine cancer statistics. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/uterine-cancer. Updated July 3, 2017. Accessed January 18, 2018.
Kitson SJ, Evans DG, Crosbie EJ. Identifying high-risk women for endometrial cancer prevention strategies: proposal of an endometrial cancer risk prediction model. Cancer Prev Res (Phila). 2017;10(1):1-13. doi:10.1158/1940-6207.CAPR-16-0224.
Castle PE, Katki HA. Screening: a risk-based framework to decide who benefits from screening. Nat Rev Clin Oncol. 2016;13(9):531-532. doi:10.1038/nrclinonc.2016.101
Girschik J, Miller LJ, Addiscott T, et al. Precision in setting cancer prevention priorities: synthesis of data, literature, and expert opinion. Front Public Health. 2017; 5:125. doi:10.3389/fpubh.2017.00125
Kotdawala P., Kotdawala S., Nagar N. Evaluation of endometrium in peri-menopausal abnormal uterine bleeding. Journal of Mid-Life Health. 2013;4(1):16–21. doi: 10.4103/0976-7800.109628.
Takreem A., Danish N., Razaq S. Incidence of endometrial hyperplasia in 100 cases presenting with polymenorrhagia/menorrhagia in perimenupausal women. Journal of Ayub Medical College: JAMC. 2009;21(2):60–63.
Nazim F., Hayat Z., Hannan A., Ikram U., Nazim K. Role of transvaginal ultrasound in identifying endometrial hyperplasia. Journal of Ayub Medical College: JAMC. 2013;25(1-2):100–102.
Ryszard B., Rzepka-Górska I. [Transvaginal ultrasonography in the diagnosis of endometrial and uterine cavity changes in perimenopausal women] Ginekologia Polska. 2002;73(11):985–990.
Bender HG. Unexpected cancer diagnosed at gynecologic surgery. Clin Obstet Gynecol. 2002; 45(2):439 -48.
Osmers R, Volksen M, Schauer A . Vaginosonography for early detection of endometrial carcinoma? Lancet. 1990; 335:669 -71.
Momtaz M, Khalil A, Al Balkini N, El Shennofi O , Mosaad M . Transvaginal sonographic characterization of endometrial hyperplasia. The journal of Egyptian society of obstetrics and gynecology. 1993; XIX(1):43.
Kelly P, Dobbs SP, McCluggage WG. Endometrial hyperplasia involving endometrial polyps: report of a series and discussion of the significance in an endometrial biopsy specimen. BJOG. 2007 ; 114(8):944 -50. Epub 2007 Jun 12.
Opmeer BC, van Doorn HC, Heintz AP. Improving the existing diagnostic strategy by accounting for characteristics of the women in the diagnostic work up for postmenopausal bleeding. BJOG. 2007 ; 114(1):51 -8.
Guner H, Tiras MB, Karabacak O, Sarikaya H, Erdema M , Ylidirim M. et al. Endometrial assessment by vaginal ultrasonography might reduce endometrial sampling in patients with postmenopausal bleeding: a prospective study, Aus N.Z.J. Obstet Gynecol. 1996; 36:175 -8.
Granberg S, Wikland M, Karlsson B, Norstrom A , Friberg L (1991): Endometrial thickness as measured by endovaginal ultrasonography for identifying endometrial abnormality. Am. J. Obstet. Gynecol. 1990; 164:47 -52.
Malinova M , Pehlivanov B . Transvaginal sonography and progesterone challenge for identifying endometrial pathology in postmenopausal women. Intern J obstet Gynecol. 1996; 52:49 -53.
Dueholm M, Marinovskij E, Hansen ES, Møller C, Ørtoft G. enopause. 2015; 22(6):616 -26 .
Krishnamoorthy N, Fatima Shanthini N. Int J Reprod Contracept Obstet Gynecol. Role of transvaginal sonography and hysteroscopy in abnormal uterine bleeding: does the diagnostic yield increase by combining transvaginal sonography, hysteroscopy and biopsy. 2014 ; 3(4):919 -92 3 .
Ramanathan R, Mancini RA, Suman SP, Beach CM. "Covalent Binding of 4 -Hydroxy - 2 -nonenal to Lactate Dehydrogenase Decreases NADH Formation and Metmyoglobin Reducing Activity." J Agric Food Chem. 2014; 62(9):2112 - 7
Xu HN, Kadlececk S, Profka H, Glickson JD, Rizi R, Li LZ. et al. "Is Higher Lactate an Indicator of Tumor Metastatic Risk? A Pilot MRS Study Using Hyperpolarized (13)C - Pyruvate.". Acad Radiol. 2014; 21(2):223 -31 .