Efficacy of zinc therapy in verruca vulgaris-A study in Shaheed Ziaur Rahman Medical College, Bogura, Bangladesh
Abstract
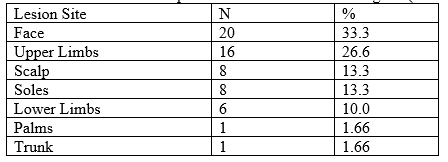
Introduction: Verruca vulgaris, caused by human papilloma virus (HPV), is a common skin condition world-wide which may be transmitted through breaks in the skin or autoinoculation into adjacent skin. The most common treatment for warts is physical destruction of the lesion. Treatment on numerous lesions using physical destruction, such as electrocautery, curettage, and cryotherapy is avoided by some patients due to pain, discomfort, recurrence and prolonged healing time. Objective: To assess the efficacy of zinc therapy in verruca vulgaris in our Dermatology outpatient department. Methods: This study was designed as a none randomized quasi experimental study including all patients above 15 years of age, who visited Skin & VD outpatient Department of Shaheed Ziaur Rahman Medical College Hospital, Bogura, Bangladesh from January to June 2022. 60 patients included in our study. Patients with mucosal warts or taking other drugs for warts or for any systemic disease for last two months to study or suffering with systemic illnesses or pregnancy and lactating were excluded for the study photographs were taken at baseline and at the outcome assessment. All patients were clinically examined thoroughly to rule out any systemic disease. Digital photographs were taken at baseline and at the outcome All data including demographic profile, clinical, response of treatment and side effects was recorded in an All patients were given Oral Zinc sulphate 10mg/kg/body weight (maximum of 600mg) daily for 3 months. Baseline investigations were carried out to rule out any systemic disease. Results: Total 60 patients were studied in this study. Mean years of presentation was 36 years. Commonest age group of presentation was seen between 15 and 25 years, 32(53.3%) patients (Table-1). Thirty (60%) patients were females. For the profession, 21(36%) patients were students. The difference between three months’ treatment of verruca vulgaris, 16.6% had 1 month, 20.0% and 63.3% had 2, 3 months respectively. Commonest site of presentation was seen over face in 20(33.3%) patients, followed by upper limbs 16(26.6%), scalp 8 (13.3%), soles 8 (13.3%), lower limbs 6 (10%), palms one (1.6%) and trunk 1 (1.6%). Mostly lesions were papules in 23 (38.3%) followed by papule and plaques in 18(30%), plaques in 12(20%) and combinations of nodules, papules and plaques in 7(11.6%). In about 27(45%) patients, lesions were firm, smooth in 25(41.6%) with regular margin in 32(53.3%). During follow-up of one month no improvement was seen in 13(21.6%), 25% improvement was seen in 36(60%), 50% improvement in 8 (13.3%) and 75% improvement in 3 (5%) patients. Side effects like nausea and mild abdominal pain was seen in 9 (10%) patients (See Table 2). Follow-up in two months showed 25% improvement in 30(50%), 50% improvement in 17(28.3%) and 75% improvement in 7(11.6%). Dropout rate was 1.66%. Side effect was seen in 1 (1.66%) patient who had gastrointestinal upset. Follow-up in three month showed 25% improvement in 15(25%), 50% improvement in 21(35%), 75% improvement in 16(26.6%) and 100% improvement in 4(6.66%) patients. This improvement over 3 months was statistically significant (p< 0.05).
Downloads
References
Skin Contact. The Official Newsletter of the Philippine Dermatological Society. March 2020; Volume 16 Number 66.
Goldsmith LA, Fitzpatrick TB (Thomas B. Fitzpatrick’s Dermatology in General Medicine.; 2012.
Lipke MM. An Armamentarium of Wart Treatments. Clin Med Res. 2006;4:273-293.
Bern B, Venge P, Ohman S: Perifolliculitis capitis abscedens et suffodeins (Hoffman). Complete healing associated with oral zinc therapy. Arch Dermatol. 1985;121:1028-30.
Johnson ML, Robert J: Skin conditions and related need for medical care among persons 1-74 years. US Department of health education and welfare publication. 1978;1660:1-26.
Beliaeva TL: The population incidence of warts. Vestn Dermatol Venerol. 1990;2:55-8.
Park HS, Choi WS: Pulsed dye laser treatment for viral warts:A study of 120 patients. J Dermatol. 2008;35:491-8.
Fraker PJ: Zinc deficiency and immune function. Arch Dermatol. 1987; 123:1699-701.
Deligeoroglou E, Giannouli A, Athanasopoulos N, et al. HPV infection: Immunological aspects and their utility in future therapy. Infect Dis Obstet Gynecol. 2013.
Sharquie K, Al-Nuaimy A. Treatment of viral warts by intralesional injection of zinc sulphate. Ann Saudi Med. 2002;22(1-2):26-28. DOI: 10.5144/0256- 4947.2002.26.
Mohamed EEM, Tawfik KM, Mahmoud AM. The Clinical Effectiveness of Intralesional Injection of 2% Zinc Sulfate Solution in the Treatment of Common Warts. Scientifica (Cairo). 2016;2016. DOI: 10.1155/2016/1082979.
Williams HC, Pottier A, Strachan D: The descriptive epidemiology of warts in British schoolchildren. Br J Dermatol 1993;128:504-11.
Kilkenny M, Merlin K, Young R, Marks R: The prevalence of common skin conditions in Australian school students: Common, plane and plantar viral warts. Br J Dermatol. 1988;138:840-5.
Fraker PJ: Zinc deficiency and immune function. Arch Dermatol. 1987;123:1699-701.
Russell RM, Suter PM: Vitamin and trace mineral deficiency and excess. In: Harrison’s principles of Internal Medicine Longo Dl, Fauci AS ,Kasper DL, Hauser SL, Jameson JL, Loscalzo J eds 18th edn. New York: Mc Graw-Hill. 2012:594-605.
11. Fraker PJ: Interrelationship between zinc and immune function. Fed Proc. 1986;45:1475.
Wirth JJ, Fraker PJ, Kierszenbaum F: Zinc requirement for macrophage function: Effect of zinc deficiency on uptake and killing of a protozoan parasites. Immunology. 1989;68:114-9.
Mahajan PM, Jadhar VH, Patki AH: Oral zinc in recurrent erythema nodosum leprosum: a clinical study. Indian J Lepr. 1994;66:51-7.
Al-Gurari FT, Al-Waiz M, Sharque KE: Oral zinc sulphate in the treatment of recalcitrant viral warts: randomized placebo controlled clinical trial. Br J Dermatol. 2002;146:423-31.