Outcome of medical induction of labour in post-dated pregnancy
Abstract
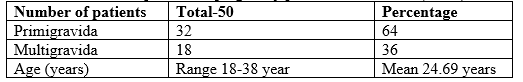
Introduction: Post maturity, post-term, Postdate, and prolonged pregnancy is accepted terms by WHO and the International Federation are of Gynecology and Obstetrics to describe pregnancy beyond dates (expected date of delivery). Prolongation of pregnancy complicates up to 10% of all pregnancies and carries increased risk to mother and foetus. Objective: To study of medical induction of labour in post-dated pregnancy. Methods: This prospective observational study was conducted in the Department of Obstetrics and Gynecology, 250 Bedded Sadar Hospital, Jhenaidah, Bangladesh from January to June 2022. Fifty (50) patients included in our study. Labour induction in post-dated pregnancy was performed only after appropriate assessment of the mother and foetus. The inclusion criteria were intact membrane, cephalic presentation, singleton pregnancies, low Bishop score in post-dated pregnancies. Absolute contraindications to induction of labour include contracted pelvis, placenta previa, unexplained vaginal bleeding, presentation other than head and previous caesarean section were excluded from the study. This study shows that the main method was oxytocin drip and second method was ARM+oxytocin in drip, some cases induced by using oral prostaglandin and very few cases induced by intra cervical prostaglandin. Results: Total 50 patients included in our study. Among than 32 patients were primigravida and 18 patients were multigravida. They were 18-38 years of age range. 20 patients (40%) were induced by only oxytocin drip and second method was ARM+oxytocin drip applied on 20 patients, some cases-7 patients (20%) were induced by using oral prostaglandin and very few cases-3 patients (10%) were induced by intra cervical prostaglandin. Only oxytocin drip and failure rate was 30%, combined ARM and oxytocin drip applied on 20 patient and failure rate was 20%. 1 patient were induced by using oral prostaglandin and failure rate was 14.2% and very few cases-3 patients were induced by intra cervical prostaglandin and failure rate was 0.0% Among spontaneous vaginal delivery was 70 %, 14% assisted vaginal delivery. Among them Forceps covers 6% and Ventouse covers 8%. 12% Caesarean section was done for foetal distress, 4% for cervical distocia and 4% for hyper stimulation. Among them healthy baby was born 70%. 26% distress baby and 4% Still birth. Conclusion: The timely onset of labour is an important determinant of perinatal outcome. Confirmation of diagnosis of postdatism is very important. In management of postdatism a careful advice and proper monitoring can alleviate maternal anxiety and untoward complications. It is a routine practice in many centers of our country to terminate most of the post-dated pregnancy by caesarean section due to limitations of foetal monitoring system and oxytocin titration Induction of labour in the presence of a ripe cervix and favorable fetal presentation appears to carry little risk to mother or foetus.
Downloads
References
WHO: recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta Obstet Gynecol Scand. 1977;56(3):247-53.
Olesen AW, Westergaard JG, Olsen J. Perinatal and maternal complications related to postterm delivery: a national register-based study, 1978-1993. Am J Obstet Gynecol. 2003;189:2227.
Norwitz ER, Snegovskikh VV, Caughey AB. Prolonged pregnancy: when should we intervene?. Clin Obstet Gynecol. 2007;50:547-57.
Eik-Nes SH, Okland O, Aure JC, Ulstein M. Ultrasound screening in pregnancy: A randomised controlled trial. Lancet. 1984;1:1347.
Ingemarsson I, Hedén L. Cervical score and onset of spontaneous labor in prolonged pregnancy dated by second-trimester ultrasonic scan. Obstet Gynecol. 1989;74:102-5
Report of the FIGO subcommittee on perinatal epidemiology and health statistics following a workshop on the methodology of measurement and recording of infant growth in perinatal period. Cairo. November 11 to 18, 1984. International Federation of Gynecology and Obstetrics (FIGO). London. Int J Gynecol Obstet. 1986;24:483.
Rayburn WF. Clinical experience with a controlled release,prostaglandin E2 intravaginal insert in the USA. Br J Obstet Gynaecol 1997; 104(Suppl 15): 8-12.
Perry KG, Larman JE,May WL, Robinette LG Martin RW. Cervical ripening: a randomized comparison between intravaginal misoprostol and an intracervical balloon cather combined with intravaginal Cinoprostonc, Ar:l ,r Obstet Gynaecol 1998; 173: 1333-40.
Ozan H, Gurkan U, Volkan Y, Fk, Mphpara T Misoprostol in labour induction. J Obstet Gynaecol Res 2001 ; 2l ; 11 -20 .
Carol L. Archie, The Course & Conduct of normal labour & delivery, Current Diagnosis & Treatment Obstetrics & Gynaecology, lOth Edition Page, 203-2ll
Jahan S ; Clinical study on Induction and outcome of lobour Dhaka BcPs 1990.
Alexander JM, McIntire DD, Leveno KJ. Prolonged pregnancy: induction of labour and caesarean births. Obstet Gynecol 2001;97:911. DOI: 10.1016/s0029-7844(01)01354-0.
Boulvain M, Stan C, Irion O. Membrane sweeping for induction of labour. Cochrane Database Syst Rev 2005;1:CD000451. DOI: 10.1002/14651858.CD000451.pub3.
Schaffir J. Survey of folk beliefs about induction of labor. Birth 2002;29:47–51. DOI: 10.1046/j.1523-536x. 2002.00047.x.
Reddy UM, KO CW, Willinger M. Maternal age and risk of stillbirth throughout pregnancy in the United States. Am J Obstet Gynecol. 2006;195(3):764-70
Shephered JH Pearce Jmf, Sims CD. Induction of lobour using prostaglandin, Br med J 1919, 2: 108-110.
Hassan Zafirul, A study on induction of lobour, IPGMR, 1995.A.
Gulmezoglu AM, Crowther CA, Middleton P. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database Syst Rev. 2012;6:CD00494.