Pregnancy outcomes of diabetic women; A single centre experience
Abstract
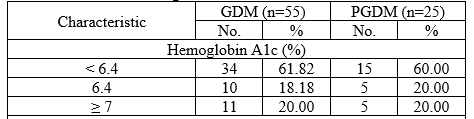
Introduction: Diabetes in pregnancy is associated with preterm delivery, birthweight extremes, and increased rates of congenital anomaly, stillbirth, and neonatal death. Aim of the study: This study aimed to determine the maternal and perinatal outcomes of diabetic pregnant women managed at Chittagong Medical College and Hospital, Chittagong Bangladesh. Methods: This retrospective case-control study was conducted at the department of Gynecology and Obstetrics Chittagong Medical College and Hospital, Chittagong Bangladesh. This study was conducted from the registry case details of women with Gestational Diabetes Mellitus (GDM) and Pre-gestational Diabetes Mellitus (PGDM) (Type-1 or Type-2) from January 2021 to December 2021. Result: A total of 133 patients were enrolled and analyzed in this study into three groups 1st Control group with 53 patients, 2nd Gestational Diabetes Mellitus (GDM) with 55 patients, and Pre-Gestational Diabetes Mellitus (PGDM) with 25 patients. There is an impact on SCBU admission; most of the babies in the control group were not admitted to SCBU, 36(65.45%) babies were not admitted, and 19(34.55%) babies were admitted to SCBU of the GDM group. Nevertheless, almost 50% of babies were admitted to SCBU of the PGDM group. Conclusion: Women with pregnancies complicated by diabetes had a higher incidence of adverse maternal and perinatal outcomes. Clinical recognition of diabetes in pregnancy is important because institution of therapy, and antepartum fetal surveillance can reduce the maternal and perinatal morbidity and mortality associated with the condition.
Downloads
References
Hossein-Nezhad A, Maghbooli Z, Vassigh AR, Larijani B. Prevalence of gestational diabetes mellitus and pregnancy outcomes in Iranian women. Taiwanese Journal of Obstetrics and Gynecology. 2007 Sep 1; 46(3):236-41.
Chang SC, O'Brien KO, Nathanson MS, Mancini J, Witter FR. Hemoglobin concentrations influence birth outcomes in pregnant African-American adolescents. The Journal of nutrition. 2003 Jul 1; 133(7):2348-55.
Ifunanya NJ, Idzuinya OB, Okwuchukwu OV, Chibuzor UD, Chukwu IC, Nobert OC, Uchenna OV. Evaluation of Pregnancy Outcomes among Women with Pregnancies Complicated by Diabetes Mellitus in Abakaliki, South-East, Nigeria. Journal of Diabetes Mellitus. 2019 Aug 9; 9(3):69-76.
Fareed P, Siraj F, Lone K. Fetomaternal outcome in women with gestational diabetes mellitus. International Journal of Research in Medical Sciences. 2017 Sep; 5(9):4151.
Frolkis JP, Pothier CE, Blackstone EH, Lauer MS. Frequent ventricular ectopy after exercise as a predictor of death. New England Journal of Medicine. 2003 Feb 27; 348(9):781-90.
Saxena P, Tyagi S, Prakash A, Nigam A, Trivedi SS. Pregnancy outcome of women with gestational diabetes in a tertiary level hospital of north India. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine. 2011 Apr; 36(2):120.
Jensen DM, Damm P, Moelsted-Pedersen L, Ovesen P, Westergaard JG, Moeller M, Beck-Nielsen H. Outcomes in type 1 diabetic pregnancies: a nationwide, population-based study. Diabetes care. 2004 Dec 1; 27(12):2819-23.
Palatnik A. 608: The association of timing of treatment initiation for mild gestational diabetes with perinatal outcomes. American Journal of Obstetrics & Gynecology. 2015 Jan 1; 212(1):S302.
Black MH, Sacks DA, Xiang AH, Lawrence JM. The relative contribution of prepregnancy overweight and obesity, gestational weight gain, and IADPSG-defined gestational diabetes mellitus to fetal overgrowth. Diabetes care. 2013 Jan 1; 36(1):56-62.
Hod, M., Kapur, A., Sacks, D.A., Hadar, E., Agarwal, M., Di Renzo, G.C., Roura, L.C., McIntyre, H.D., Morris, J.L. and Divakar, H., 2015. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: A pragmatic guide for diagnosis, management, and care. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics, 131, pp.S173-S211.
Feig DS, Hwee J, Shah BR, Booth GL, Bierman AS, Lipscombe LL. Trends in incidence of diabetes in pregnancy and serious perinatal outcomes: a large, population-based study in Ontario, Canada, 1996–2010. Diabetes care. 2014 Jun 1; 37(6):1590-6.
Mackin ST, Nelson SM, Kerssens JJ, Wood R, Wild S, Colhoun HM, Leese GP, Philip S, Lindsay RS. Diabetes and pregnancy: national trends over 15 years. Diabetologia. 2018 May; 61(5):1081-8.
Radder JK, Van Roosmalen J. HbA1c in healthy, pregnant women. Neth J Med. 2005 Jul 1; 63(7):256-9.
Balsells M, Garcia-Patterson A, Gich I, Corcoy R. Maternal and fetal outcome in women with type 2 versus type 1 diabetes mellitus: a systematic review and meta-analysis. The Journal of Clinical Endocrinology & Metabolism. 2009 Nov 1; 94(11):4284-91.
Dunne F, Brydon P, Smith K, Gee H. Pregnancy in women with type 2 diabetes: 12 years outcome data 1990–2002. Diabetic Medicine. 2003 Sep; 20(9):734-8.
Murphy HR, Bell R, Cartwright C, Curnow P, Maresh M, Morgan M, Sylvester C, Young B, Lewis-Barned N. Improved pregnancy outcomes in women with type 1 and type 2 diabetes but substantial clinic-to-clinic variations: a prospective nationwide study. Diabetologia. 2017 Sep; 60(9):1668-77.
Mackin ST, Nelson SM, Wild SH, Colhoun HM, Wood R, Lindsay RS. Factors associated with stillbirth in women with diabetes. Diabetologia. 2019 Oct; 62(10):1938-47.
Macintosh MC, Fleming KM, Bailey JA, Doyle P, Modder J, Acolet D, Golightly S, Miller A. Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: a population-based study. BMJ. 2006 Jul 20; 333(7560):177.
Murphy HR, Steel SA, Roland JM, Morris D, Ball V, Campbell PJ, Temple RC, East Anglia Study Group for Improving Pregnancy Outcomes in Women with Diabetes (EASIPOD). Obstetric and perinatal outcomes in pregnancies complicated by Type 1 and Type 2 diabetes: influences of glycaemic control, obesity and social disadvantage. Diabetic Medicine. 2011 Sep; 28(9):1060-7.
Mathew M, Machado L, Al-Ghabshi R, Al-Haddabi R. Fetal macrosomia. Risk factor and outcome. Saudi medical journal. 2005 Jan 1; 26(1):96-100.
Shahida A. Abnormal glucose screening test followed by normal glucose tolerance test and pregnancy outcome.
El Mallah KO, Narchi H, Kulaylat NA, Shaban MS. Gestational and pre-gestational diabetes: comparison of maternal and fetal characteristics and outcome. International Journal of Gynecology & Obstetrics. 1997 Aug 1; 58(2):203-9.
Misra R, Rashid N, Grundsell H, Sedagathian MR. Clinical Forum Diabetes Mellitus in Pregnancy: The United Arab Emirates Experience. Int J Diabetes & Metabolism. 2001; 9:32-7.
Shefali AK, Kavitha M, Deepa R, Mohan V. Pregnancy outcomes in pre-gestational and gestational diabetic women in comparison to a non-diabetic women-A prospective study in Asian Indian mothers (CURES-35). Journal of the Association of Physicians of India. 2006; 54:613-8.
Abolfazl M, Hamidreza TS, Narges M, Maryam Y. Gestational diabetes and its association with unpleasant outcomes of pregnancy. Pak J Med Sci. 2008 Jul 1; 24(4):566-70.
Barakat MN, Youssef RM, Al-Lawati JA. Pregnancy outcomes of diabetic women: charting Oman’s progress towards the goals of the Saint Vincent Declaration. Annals of Saudi medicine. 2010 Jul; 30(4):265-70.
Boriboonhirunsarn D, Lertbunnaphong T, Tientong K. Diagnosis of gestational diabetes mellitus: comparison between National Diabetes Data Group and Carpenter–Coustan criteria. Asian Biomedicine. 2014 Aug 1; 8(4):505-9.
De Valk HW, van Nieuwaal NH, Visser GH. Pregnancy outcome in type 2 diabetes mellitus: a retrospective analysis from the Netherlands. The Review of Diabetic Studies. 2006; 3(3):134.
Jensen DM, Sørensen B, Feilberg‐Jørgensen N, Westergaard JG, Beck‐Nielsen H. Maternal and perinatal outcomes in 143 Danish women with gestational diabetes mellitus and 143 controls with a similar risk profile. Diabetic medicine. 2000 Apr; 17(4):281-6.
Holan S, Vangen S, Hanssen K, Stray-Pedersen B. Pregnancy in diabetes among Asian, African and Norwegian women. Tidsskrift for den Norske Laegeforening: Tidsskrift for Praktisk Medicin, ny Raekke. 2008 May 1; 128(11):1289-92.
Tanir HM, Sener T, Giirer H, Kaya M. A ten-year gestational diabetes mellitus cohort at a university clinic of the mid-Anatolian region of Turkey. Clinical and experimental obstetrics & gynaecology. 2005 Dec 10; 32(4):240-4.
Conway DL. Obstetric management in gestational diabetes. Diabetes Care. 2007 Jul 1; 30(Supplement_2):S175-9.
Watson D, Rowan J, Neale L, Battin MR. Admissions to neonatal intensive care unit following pregnancies complicated by gestational or type 2 diabetes. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2003 Dec; 43(6):429-32.
Clausen TD, Mathiesen E, Ekbom P, Hellmuth E, Mandrup-Poulsen T, Damm P. Poor pregnancy outcome in women with type 2 diabetes. Diabetes care. 2005 Feb 1; 28(2):323-8.