Peroperative renal pain lower in upper spinal block of proximal (upper) ureteric stone management by URS + ICPL under spinal anesthesia
Abstract
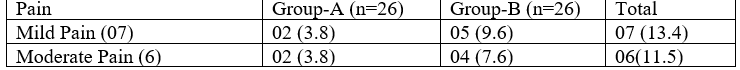
Introduction: Proximal (upper) Ureteric stone management by URS + ICPL under Spinal Anesthesia; Upper Spinal Block (USAB) reduces / lowers the Renal pain than Lower Spinal Block (LSAB). Objective: To ensure patients compliance and or to reduce renal and flank pain due to high irrigation fluid pressure and or due to rigid ureteroscopy through ureter during URS + ICPL of Upper ureteric stone operation under Spinal Anesthesia. Material & Methods: Randomized prospective study of 60 patients admitted in National Institute of Kidney Diseases & Urology (NIKDU), Dhaka, Bangladesh from early January 2019 to late January 2020 with the diagnosis of proximal (upper) ureteric stone for URS + ICPL under Spinal Anesthesia. Demographic study of the patients age, sex, ASA Score having no spinal deformity. Every patient was properly informed & counselled about the whole procedures & outcomes including Spinal anesthesia (SAB) and URS +ICPL. Written informed consent was taken from all patients and their legal guardians as well. Patients with contraindications to SAB (Coagulopathy, local infection. etc.), allergies to local anesthetic sol, opioids, drugs used, and significant spine, hepatic, cardiovascular, respiratory or psychiatric disorders were excluded from the study. Results: 60 patients were randomly selected of which 30 pt's selected for Group-A and 30 pt's for Group B. Finally, 26 patients in each Group i.e., total 52 patients were done URS+ICPL under SAB subject for our study. 13 Patients had complained of mild to moderate pain (VAS: 0-6) of which 4 patients Group: A and 9 patients Group: B. In Group: A; 2 of 4 pt's had complained of mild pain (VAS:<3) and required analgesic i.e., Inj ketorolac 30mg IV & 2 pt's had complained of moderate pain (VAS: >3-6) required potent analgesic i.e., Inj Pethidine 50mg IV slowly in addition to Inj ketorolac 30mg. In Group: B; 5 of 9 pt's had complained of mild pain (VAS:<3) and required analgesic i.e. Inj ketorolac 30mg IV & 4 pt's had complained of moderate pain (VAS:>3-6) required potent analgesic i.e. Inj pethidine 50mg IV slowly in addition to IV Inj ketorolac 30mg. 8 patients had developed hypotension of which 6 in Group: A where 3 pt's had developed moderate hypotension and required vasopressor (Inj Ephedrine HCl 10-30mg) with the increased IV fluid respectively & 3 pt's had developed mild hypotension hadn't got vasopressor but got increased IV fluid. And 2 pt's in Group: B had developed mild hypotension hadn't gotten any vasopressor but got increased IV fluid. 5 Patients had developed bradycardia (HR: >45-60 beat/min) of which 4 in Group: A & 1in Group: B had required inj Atropine 0.3-0.6mg. 14 Patients had developed tachycardia (HR: >90 beat/min) of which 5 in Group: A & 09 in Group: B. The tachycardia was usually accompanied by pain during procedures & little with hypotension. 3 Patients developed little anorexia without vomiting of only Group: A & neither of Group: B following moderate hypotension & bradycardia which were managed respectively.
Downloads
References
Reis Santos JM. Ureteroscopy from the recent past to the near future. Urolithiasis. 2018; 46: 31-37.
Coll DM, Varanelli MJ, Smith RC. Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. AJR Am J Roentgenol. 2002; 178: 101-103.
Türk C, Neisius A, Petrik A, Seitz C, Thomas K. Guidelines on urolithiasis. European Association of Urology, Arnhem 2018. Available at http://www.uroweb.org/gls/pdf.
Moon, K.T., Cho, H.J., Cho, J.M., Kang, J.Y., Yoo, T.K., Moon, H.S. and Lee, S.W., 2011. Comparison of an indwelling period following ureteroscopic removal of stones between Double-J stents and open-ended catheters: a Prospective, pilot, randomized, multicenter study. Korean journal of urology, 52(10), pp.698-702.
Netto, N.R., Ikonomidis, J. and Zillo, C., 2001. Routine ureteral stenting after ureteroscopy for ureteral lithiasis: is it really necessary?. The Journal of urology, 166(4), pp.1252-1254
Harmon WJ, Sershon PD, Blute ML, Patterson DE, Sequra JW. Ureteroscopy: currentpractice and long-termcomplications. J Urol 1997; 157: 28-32.
Maghsoudi R, Amjadi M, Norizadeh D, Hassanzadeh H. Treatment of ureteral stones: A prospective randomized controlled trial on comparison of Ho:YAG laser and pneumatic lithotripsy. Indian J Urol 2008; 24(3): 352–354. doi: 10.4103/0970-1591.39549.
NettoJunior NR, ClaroJde A, Esteves SC, Andrade EF. Ureteroscopics tone removal in the distalureter. Whychange? J Urol 1997; 157: 2081-3. 8. Wills TE, Burns JR. Ureteroscopy: an outpatient procedure? J Urol 1994; 151: 1185-1187.
Rittenberg MH, Ellis DJ, Bagely DH. Ureteroscopy under local anaesthesia. Urology 1987; 30: 475-478.
Vogelli A, Mellin HE, Hopf B, Ackermann R. Ureteroscopy under local anaesthesia with and without intravenous analgesia. Br J Urol 1993; 72: 161-164
Chauhan, V.S., Bansal, R. and Ahuja, M., 2015. Comparison of efficacy and tolerance of short-duration open-ended ureteral catheter drainage and tamsulosin administration to indwelling double J stents following reteroscopic removal of stones. Hong Kong Med J, 21(2), pp.124-30.
alçinkaya F, Topaloğlu H, Ozmen E, Unal S. Is general anesthesia necessary for URS in women? Int Urol Nephrol. 1996;28:153–156.
Large T, Heiman J, Ross A, Anderson B, Krambeck A. Initial experience with narcotic-free ureteroscopy: a feasibility analysis. J Endourol. 2018;32:907–911.
Hosking DH, Smith WE, McColm SE. A comparison of extracorporeal shock wave lithotripsy and ureteroscopy under intravenous sedation for the management of distal ureteric calculi. Can J Urol. 2003;10:1780–1784.