Supraclavicular brachial plexus block using 0.5% bupivacaine with and without fentanyl
Abstract
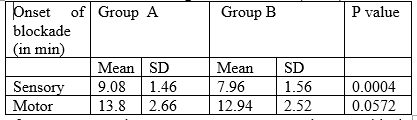
Introduction: Brachial plexus block is good alternative to general anesthesia for upper limb surgery. This avoids the unwanted effect of anesthetic drugs used during general anesthesia and the stress of upper airway instrumentation. Objective: To assess the supraclavicular brachial plexus block using 0.5% bupivacaine with and without fentanyl. Materials and Methods: This study design was a prospective randomized controlled double-blinded clinical study was carried out at Department of Anaesthesiology, Shaheed M. Monsur Ali Medical College and Hospital, Sirajganj, Bangladesh from January to June 2021. Fifty (50) patients with American Society of Anesthesiologists physical status Classes I and II, aged 18–50 years, scheduled for upper limb surgery were randomly divided into Two study groups each group contains 25 patients: A Group: receive 0.4 ml/kg bupivacaine up to a maximum of 30 ml volume plus 1ml of normal saline. The dose of bupivacaine was 2 mg/kg. B Group: Bupivacaine as control group plus 1 mcg/kg fentanyl. Patients were excluded if they had sepsis at the site of injection, body wt<50kg, pregnant women, known hypersensitivity, circulatory instability, diabetes, coagulopathy, history of neurological, renal & liver diseases, mental disease and malignancy. Results: Total 50 patient were included both groups. The groups were comparable with respect to age, height, and weight, and ASA physical status. There was no significant difference in the type and duration of surgery. The characteristics of sensory block are summarized. Demographic characteristics and duration of surgery were comparable in both the groups and the difference was not statistically significant (p>0.05). Duration of sensory and motor blockade was longer in group B and shorter in group A. The differences in duration of sensory and motor blocks were statistically significant in both groups. Pulse rate, blood pressure, oxygen saturation was monitored throughout the surgery and also postoperatively. All values were within the normal range. There was no statistically significant difference between the mean preoperative, intra-operative and postoperative values. The vitals were well maintained in all the patients. The timing of the first rescue analgesia was significantly late and the total consumption of analgesia was significantly less in the first 24 hours in Bupivacaine group. Conclusion: Supraclavicular brachial plexus block using local anesthetic, with or without fentanyl revealed that addition of fentanyl to bupivacaine significantly causes early onset of anesthesia and longer duration of analgesia without any side effects. On the basis of the results of the present study, integrated with understanding from the available literature it may be recommended that, this technique will open new perspective for upper limb surgery under regional anesthesia.
Downloads
References
Wakhlo R, Gupta V, Raina A, Gupta SD, Lahori VU. Supraclavicular brachial plexus block: Effect of adding tramadol or butorphanol as an adjuncts to local anaesthetic on motor and sensory block and duration of postoperative analgesia. J Anaesthesiol Clin Pharmacol 2009;25:17 20.
Iohom G, Machmachi A, Diarra DP, Khatouf M, Boileau S, Dap F, et al. The effects of clonidine added to mepivacaine for paronychia surgery under axillary brachial plexus block. Anesth Analg 2005;100:1179 83.
Lalla RK, Anant S, Nanda HS. Verapamil as an adjunct to local anaesthetic for brachial plexus blocks. Med J Armed Forces India 2010;66:22 4.
Benzone HT. Epidural steroid. In: Raj PP, editor. Pain Medicine: A Comprehensive Review. UK: Mosby publication; 1999. p. 259 63.
Elhakim M, Ali NM, Rashed I, Riad MK, Refat M. Dexamethasone reduces postoperative vomiting and pain after pediatric tonsillectomy. Can J Anaesth 2003;50:392 7
El-Emam E-SM. Comparative evaluation of dexamethasone and dexmedetomidine as adjuvants for bupivacaine in ultrasound Guided infraorbital nerve block for cleft lip repair: A prospective, randomized, Double-Blind study. Anesthesia, essays, and researches. 2019; 13(2):354.
Pöpping DM, Elia N, Marret E, Wenk M, Tramer MR. Clonidine as an Adjuvant to Local Anesthetics for Peripheral Nerve and Plexus BlocksA Meta-analysis of Randomized Trials. Anesthesiology: The Journal of the American Society of Anesthesiologists. 2009;111(2):406-15.
Rachel H, Foster AM. Levobupivacaine A Review of its pharmacology and use as a Local Anaesthetic. Drugs. 2000;59(3):551.
Saryazdi H, Yazdani A, Sajedi P, Aghadavoudi O. Comparative evaluation of adding different opiates (morphine, meperidine, buprenorphine, or fentanyl) to lidocaine in duration and quality of axillary brachial plexus block. Advanced biomedical research. 2015;4.
Nancheva J, Andonovski A, Georgieva D, Božinovski Z, Džoleva R, Gavrilovski A, et al. Does the addition of dexamethasone to local anesthetic prolong the analgesia of interscalen plexus brachialis block in patients with shoulder surgery? Sanamed. 2016;11(1):15-20.
Eker HE, Cok OY, Aribogan A, Arslan G. Management of neuropathic pain with methylprednisolone at the site of nerve injury. Pain Medicine. 2012;13(3):443-51.
Murphy DB, McCartney CJ, Chan VW. Novel analgesic adjuncts for brachial plexus block: A systematic review. Anesth Analg. 2000;90:1122–8.
Brummett CM, Hong EK, Janda AM, Amodeo FS, Lydic R. Perineural dexmedetomidine added to ropivacaine for sciatic nerve block in rats prolongs the duration of analgesia by blocking the hyperpolarization-activated cation current. Anesthesiology. 2011;115:836–43.
Choi S, Rodseth R, McCartney C. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials. British journal of anaesthesia. 2014;112(3):427-39.
Shrestha B, Maharjan S, Shrestha S, Gautam B, Thapa C, Thapa P, et al. Comparative study between tramadol and dexamethasone as an admixture to bupivacaine in supraclavicular brachial plexus block. JNMA J Nepal Med Assoc. 2007;46(168):158-64.
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain Intensity on the first day after surgerya prospective cohort study comparing 179 surgical procedures. Anesthesiology: The Journal of the American Society of Anesthesiologists. 2013;118(4):934-44.
Islam S, Hossain M, Maruf A. Effect of addition of dexamethasone to local anaesthetics in supraclavicular brachial plexus block. Journal of Armed Forces Medical College, Bangladesh. 2011;7(1):11-4.
Abdallah FW, Johnson J, Chan V, Murgatroyd H, Ghafari M, Ami N, et al. Intravenous Dexamethasone and Perineural Dexamethasone Similarly Prolong the Duration of Analgesia After Supraclavicular Brachial Plexus Block: A Randomized, Triple-arm, Double-Blind, placebo-Controlled Trial. Regional Anesthesia & Pain Medicine. 2015;40(2):125-32.
Singh SP, Singh V, Kaushal D, Jafa S. Comparison of Fentanyl-bupivacaine and Alkalinised bupivacaine in Supraclavicular brachial plexus block : A double blind, randomized controlled trial. Available from:http://www.aja-online.com.pdf.
Kardash K, Schools A, Conception A. E¬ects of brachial plexus fentanyl on supraclavicular block; A randomized double blind study. Reg Anes. 1995; 20: 311-5.
Hickey R, Rowley C, Candido K. A comparative study of 0.25% ropivacaine and 0.25% bupivacaine for brachial plexus block. Anesth Analg 1992; 75: 602-6.
Farooq N, Singh RB, Sarkar A, Rasheed MA, Choubey S. To evaluate the efficacy of fentanyl and dexmedetomidine as adjuvant to ropivacaine in brachial plexus block: A double-blind, prospective, randomized study. Anesth Essays Res. 2017;11:730–9.
Manohar P, Prakash M. Comparison of the effects of fentanyl and dexmedetomidine in supraclavicular brachial plexus block achieved with 0.5% bupivacaine. JMSCR. 2015;3:7131–8.
Albrecht E, Kern C, Kirkham K. A systematic review and meta‐analysis of perineural dexamethasone for peripheral nerve blocks. Anaesthesia. 2015;70(1):71-83.
Vieira PA, Pulai I, Tsao GC, Manikantan P, Keller B, Connelly NR. Dexamethasone with bupivacaine increases duration of analgesia in ultrasound-guided interscalene brachial plexus blockade. European Journal of Anaesthesiology. 2010; 27(3):285-288.