Assessment of temporomandibular disorder using Fonseca questionnaire and its classification based on DC/TMD criteria in tertiary hospital in Nepal.
Abstract
Background and objective: Temporomandibular disorders (TMD) is an orofacial disorder, associated with temporomandibular joint (TMJ) pain, masticatory muscles fatigueness, restricted mouth opening and clicking. The Fonseca anamnestic index (FAI) is questionnaire for evaluating severity and characteristics of TMD. The Diagnostic criteria for temporomandibular disorders (DC/TMD) is used for diagnosis of TMD. The study assessed the severity, clinical characteristic and patterns of TMDs in Eastern Nepal population.
Methods: A cross sectional study was done in Department of Oral Medicine and Radiology using census sampling. Eighty patients having TMD was interviewed using Fonseca's questionnaire, on pain TMJ pain, head, chewing, parafunctional habits etc. The clinical examination was done using DC/TMD examination form. The TMD was classified as pain disorder and TMJ disorder of right and left side. Statistical analysis was performed using SPSS version 11.5.
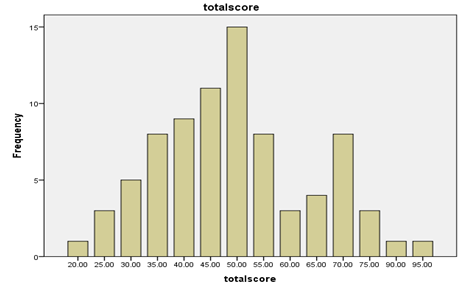
Results: FAI revealed TMD to be higher in female than male with odds ratio of 1.74. The mean age of the patient was 31.03 (±13.31). The duration from onset to diagnosis was 5.72 (±9.54) months. The Fonseca’s questionnaire showed 51.3% had moderate TMD followed by mild and severe. DCTMD criteria location of pain was most commonly in the TMJ region 47(58.8%) of cases followed by 7.5% in temporalis, masseter and other muscle and 1 (1.3%) had pain in sternocleidomastoid.
Conclusions: The TMDs showed moderate severity with Anamnestic Index. Myalgia was the most common pain disorder and disc displacement with reduction in right and left TMJ disorder.
Downloads
References
LeResche L, Saunders K, Von Korff MR, Barlow W, Dworkin SF. Use of exogenous hormones and risk of temporomandibular disorder pain. Pain 1997:69:153-60.
Bonjardim LR, Gavião MB, Pereira LJ, Castelo PM, Garcia RC. Signs and symptoms of temporomandibular disorders in adolescents. Brazilian Oral Research 2005;19: 93-98.
Garcia AL, Lacerda NJ, Pereira SLS. Evaluation of the degree of dysfunction of the temporomandibular joint and of mandibular movements in young adults. Rev Assoc Paul Cir Dent 2001;51:46-51.
Pedroni CR, De Oliveira AS, Guaratini MI. Prevalence study of signs and symptoms of temporomandibular disorder s in university students. Journal of Oral Rehabilitation 2003;30: 283-289.
Rugh JD & Solberg WK. Oral Health status in United Stated: Temporomandibular Disorders. Journal Of dental Education 1985; 49: 398-405.
Schiffman E, Fricton JR. Epidemiology of TMJ and craniofacial pain: diagnosis and management, In: The TMJ disorders management of the craniomandibular complex. New York, Churchill Livingstone, 1998.
Gray RJ, Davies SJ, Quayle AA. A clinical approach to temporomandibular disorders. Brazilian Dental Journal 1994; 176: 429-435.
Bagis B, E A Ayaz, S Turgut, R Durkan, M Ozcan. Gender difference in prevalence of signs and symptoms of temporomandibular joint disorders: a retrospective study on 243 consecutive patients. International journal of medical sciences 2012; 9(7): 539–44.
Sessle & Barry J (2014).Newly Developed Diagnostic Criteria for Temporomandibular Disorders. Journal of Oral & Facial Pain and Headache 2014;28(1):6-27.
Bonjardim LR, Lopes-Filho RJ,Amado G, Albuquerque RL, Goncalves SR. Association between symptoms of temporomandibular disorders and gender, morphological occlusion, and psychological factors in a group of university students. Indian Journal of Dental Research 2009; 20(2): 190–4.
Cooper, B.C. & Kleinberg, I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. Journal of craniomandibular practice 2007; 25(2): 114–26.
LeResche. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Critical reviews in oral biology and medicine. American Association of Oral Biologists 1997; 8(3): 291–305.
Liu, F & Steinkeler, A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dental clinics of North America 2013; 57(3): 465–79.
Nomura K, Vitti M, de Oliveira AS, CC Thais, Semprini M, Siessere S. Use of the Fonseca’s Questionnaire to Assess the Prevalence and Severity of Temporomandibular Disorders in Brazilian Dental Undergraduates. Brazilian Dental Journal 2007; 18(2): 163-167.
Otuyemi O.D, Ototade F. J, Ugboko VI, Ndukwe KC, Olusile OA. Prevalence of signs and symptoms of temporomandibular disorders in young Nigerian adults. Journal of Orthodontics 2000; 27(1): 61-65.
Shiau Y-Y, Chang C . An epidemiological study of temporomandibular disorders in university students of Taiwan. Community Dent Oral Epidemiol 1992; 20: 43-7.
Santos Berni KC, Dibai-Filho AV, Bigaton DR. Accuracy of the Fonseca anamnestic index in the identification of myogenous temporomandibular disorder in female community cases, Journal of Bodywork & Movement Therapies 2015; 19: 404- 409.
Tallents, RH. Prevalence of missing posterior teeth and intraarticular temporomandibular disorders. The Journal of prosthetic dentistry 2000; 87(1): 45–50.
Wang, MQ, Xue F, He JJ, Chen JH, Chen CS, Raustia A. Missing posterior teeth and risk of temporomandibular disorders. Journal of dental research 2009; 88(10): 942–5.
Martínez CC. Prevalence of temporomandibular disorders according to RDC/TMD, in patients of asub-urban community of Puebla, Mexico. Columbian Journal of Dental Research 2013; 4: 10-14.
Manfredini D, Chiappe G & Bosco M. Research diagnostic criteria for temporomandibular disorders (RDC/TMD) axis I diagnoses in an Italian patient population. Journal of Oral Rehabilitation 2006; 33(8): 551-8.
Yap A, Sworkin S, Chuba E, Tan K, Tan H. Prevalence of temporomandibular disorder subtypes, psychological distress, and psychosocial dysfunction in Asian patients. Journal of Orofacial Pain 2003; 17: 586-587.
Fonseca DM. Disfunção Craniomandibular. Diagnostic pela anamneses, Faculdade de Odontologia de Bauru da USP 1992; 16-23.
Bevilaqua D, Chaves T, Oliveira A, Monteiro V. Anamnestic index severity and signs and symptoms of temporomandibular disorder. Craniomandibular 2006; 24: 112–18.
Fonseca DM, Bonfante G, Valle AL, Freitas SF. Diagnóstico pela anamnese da disfun- ção craniomandibular 1994; 42(1): 23-8.
Berni, Dibai-Filho & Rodrigues-Bigaton. Accuracy of the Fonseca anamnestic index in the identification of myogenous temporomandibular disorder in female community cases. Journal of body work and therapies 2015; 19:404-409.
Wiese M, Svensson P, Bakke M, List T, Hintze H, Petersson A et al. Association between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. Oral Surgery Oral Medicine Oral Pathology Oral Radiology Endodontic 2009; 108(3): 117-24.
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the international RDC/TMD consortium network and orofacial pain special interest group dagger. J Oral Facial Pain Headache 2014; 28: 6–27.
Vilanova LRS et al. (2015) Diagnostic criteria for temporomandibular disorders: self-instruction or formal training and calibration? The Journal of Headache and Pain.2015;12:16-26.
Casanova-Rosado, J., Medina-Solís, C., Vallejos-Sánchez, A., Casanova-Rosado, A., Hernández-Prado, B., Ávila-Burgos,L. Prevalence and associated factors for temporomandibular disorders in a group of Mexican adolescents and young adults. Clin Oral Invest 2006; 10: 42-49.
Uhač, I., Kovač, Z., Valentić-Peruzović, M., Juretić, M., Moro, L., Gržić, R. The influence of war stress on the prevalence of signs and symptoms of temporo mandibular disorders. J Oral Rehab 2003:30;211-217.
Nekora-Azak, A., Evlioglu, G., Ordulu, M., Issever, H. Prevalence of symptoms associated with temporomandibular disorders in a Turkish population. J Oral Rehabil. 2006; 33: 81-84.
Pedroni, C., De Oliveira, A., Guaratini, M. Prevalence study of signs and symptoms of temporomandibular disorders in university students. J Oral Rehabil 2003; 30: 283-289.
Dekon SFC, Fajardo RS, Zavanelli AC, Beleeiro RP, Pelisser J. Estudo comparativo entre índice anamnético de DTM e inventário de ansiedade traço-estado (IDATE). JBA: J Bras Oclusão, ATM Dor Orofac 2002; 2(7): 224-7.
Pedroni CR, Oliveira AS, Guaratini MI. Prevalence study and symptoms of temporomandibular disorders in university students. J Oral Rehabil 2003; 30(2): 283-9.
Kuttila M, Kuttila S, Niemi PM, Alanen P, Le Bell Y. Fluctuation of treatment need for temporomandibular disorders and age, gender, stress, and diagnostic subgroup. Acta Odontol Scand 1997; 55(6): 350-5.
List T and Dworkin SF. Comparing TMD diagnoses and clinical findings at Swedish and US TMD centers using research diagnostic criteria for temporomandibular disorders. J Orofac Pain 1996; 10: 240–253.
Schiffman EL, Truelove EL, Ohrbach R, et al. The research diagnostic criteria for temporomandibular disorders. Overview and methodology for assessment of validity. J Orofac Pain 2010; 24: 7–24.
Anastassaki Kohler A, Hugoson A and Magnusson T. Prevalence of symptoms indicative of temporomandibular disorders in adults: Cross-sectional epidemiological investigations covering two decades. Acta Odontol Scand 2012; 70: 213–223.
List T, Wahlund K, Wenneberg B, et al. TMD in children and adolescents: Prevalence of pain, gender differences, and perceived treatment need. J Orofac Pain 1999; 13: 9–20.
Slade GD, Ohrbach R, Greenspan JD, et al. Painful temporomandibular disorder: Decade of discovery from OPPERA studies. J Dental Res 2016; 95: 1084–1092.