Maternal and Perinatal Outcome of Liver Function in Severe Pre Eclampsia and Eclampsia Patients
Abstract
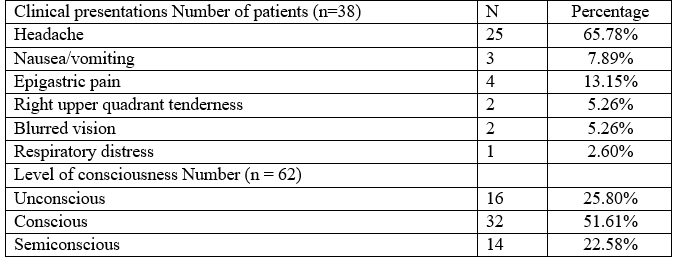
Background: Preeclampsia and eclampsia are common pregnancy specific multi system disorder in Bangladesh and are major causes of maternal, foetal and neonatal mortality and morbidity. Objective: To determine the extent of hepatic involvement in severe preeclampsia & eclampsia and its relation to fetomaternal outcome. Methods: It was a hospital based prospective study. This randomized clinical trial was conducted to evaluate liver function in severe preeclampsia and eclampsia on 100 patients with severe preeclampsia and eclampsia selected randomly who were admitted in department of obstetrics and gynaecology unit of Rangpur medical college and hospital through outpatient department and emergency during a time period of June 2015 to November 2015. Data was collected in preformed questionnaires after taking written informed consent from the patient or legal guardian after proper counseling.Then date was presented in graph and tabulated form and finally analyzed by SPSS version–16. Results: 100 patients were taken in this study–62 as eclampsia and 38 as severe preeclampsia. 0ut of 100 patients maximum (60%) were between 20-35 years of age, 62% patients were primigravida, 46% were more than 36 weeks of gestation, 53% patients were belonged to low socioeconomic status, 59% patients were primarily educated, 25% patients had no antenatal checkup and 42% were on irregular antenatal checkup. Most of the severe preeclamptic patients presented on admission with headache (65.78%) and epigastric pain (13.15%) and most of the eclamptic patient (51.61%) were conscious and 29.03% were unconscious. Maximum patients (56%) were delivered by LSCS. In severe preeclampsia group blood urea were raised in 73.68%, S. Creatinine were raised in 71.05% and S.Uric acid were raised in 65.78%. Liver function was abnormal in 21.05% patients among them S.bilirubin was raised in 15.7%, SGPT was raised in 21.05% patients SGOT was raised in 18.42% patients. LDH was raised in 13.15% patients. In eclamptic patients’ blood urea was raised in 72.58% patients, S. creatinine was raised in 66.12% patients; S. uric acid was raised in 61.29% patients. Liver function was abnormal in 22.58% patients, among them, S. bilirubin was raised in 29.03%, SGPT in 48.38%, SGOT was raised in 30.64% and LDH was raised in 45.16% patients. Maternal morbidity and mortality was more in patients with abnormal liver function. It maternal mortality was 12.5% in severe preeclamptic patients and 14.28% in eclamptic patients with abnormal liver function. Perinatal morbidity and mortality was also higher in patients with abnormal liver function. Perinatal mortality was 62.5% in severe preeclamptic patients and 42.85% in eclamptic patients with abnormal liver function. Conclusion: From this study it was found that abnormal liver function in patients with severe preeclampsia and eclampsia, affect both maternal and fetal outcome negatively. Therefore, prior information of liver function in such patients may help to reduce maternal and perinatal mortality and morbidities.
Downloads
References
Bangladesh Maternal Mortality and Health Care Survey (BMMS) 2010.
Dhananjay B.S, Dayananda G, Sendilkumeran D, Murthy N. A study of factors affecting perinatal mortality in eclampsia. JPBS.2009; 22(2): 2-5.
Munazza B, Raza N, Naureen A, Khan SA, Fatima F, Ayub M.et.al. Liver function test in pre-eclampsia. J Ayub Med Coll Abbottabad; 2011; 23(4):3-5.
Bhowmik DK, Akhtari R, Kumer SU, Saha M, Adhikari DK. Alteration of liver function in pre eclampsia and eclampsia. Chattagram Maa-o-shishu Hospital Medical College Journal 2013; Seotember. 12(3):9-10.
Sachan R, Patel ML, Sachan P, Gaurav A, Sing M, Bansal B. Outcome in hypertensive disorder in pregnancy in the North Indian population. International Journal of Women's Health; 2013:5.
Shamsi U , Saleem S, Nishter N. Epidemiology and risk factors of pre-eclampsia; An overview of observational studies. Al Ameen J Med Sci; 2013; 6(4): 292-300.
Wandabwa J, Doyle P, Kiondo P, Campbell O, Maconichie N, Welishe G. Risk factors for severe pre-eclampsia and Eclampsia In Mulago Hospital, Kampala, Uganda. East African Medical Journal 2010; October. 87(10):415-424.
Arshad A, Pasha W, Khattak T.A, Kiyani RB. Impact of pregnancy induced hypertension on birth weight of new born at term. Journal of Rawalpindi Medical college(JRMC); 2011;15(2): 113-115.
Kishwara S, Tanira S, Omar E, Wazed F, Ara S. Effect of preeclampsia on perinatal outcome- A study done in the specialized urban hospital set up in Bangladesh. Bangladesh Medical Journal.2011. 40(1):33-36.
Begum MR, Begum A, Quadir E, Akhter S, Shamsuddin L. Eclampsia: Still a problem in Bangladesh. Med. Gen. Med 2004;6(4):52.
Yaliwal RG, Jaja PB, Nanishree M, Eclampsia and perinatal outcome: A retrospective study in ateaching Hospital. Journal of Clinical and Diagnostic Research;2011. October.5(5): 1056-1059.
Alonso L.A.G. Effect of pregnancy on preexisting liver disease, Physiological change during pregnancy. Annals of Hepatology 2006; July- September; 5(3): 184-186.
Das S, Char D, Sarker S, Shaha TK, Biswas S, Rudra B. Evaluation of liver function test in Normak Pregnancy and pre-eclampsia: A Case Control. Iosr Journal of Dental and Medical Sciences (IOSR-JDMS);2013; Nov.- Dec.12(1):30-32.
Guntupalli SR, Steingrub J. Hepatic disease and pregnancy: An overview of diagnosis and management. Crit. care Med 2005;33(10): S332-S339.
Girling J.C, Dow E, Smith JA. Liver function test in pre eclampsia: importance of comparison with a reference range desired for normal pregnancy. British Journal of Obstetrics and Gynecology 2005;104(2):246-250.
Jameil NA, Tabassum H, Mayouf HA, Otay LA, Khan FA. Liver Function Tests as Probable Markers Of Pre eclampsia- A Prospective Study Conducted in Riyadh, Journal of Clinical and Analytical Medicine 2013.
Decherney A.H, Nathan L. CURRENT diagnosis and treatment Obstetrics and Gynecology .10th edit. Network. 2007;320-326.
Akter R, Ferdous A, Bhuiyan SN. Maternal and fetal outcome of eclamptic patients in a tertiary hospital. Bangladesh J Obstet Gynaecol, 2011;26(2):77-80.
Paneri S, Panchonia A, Varma M, Yadav S. Evaluation of RFTS, LFTS, and ascorbic acid in preeclampsia among women of Indore. Indian Journal of Fundamental and Applied life sciences ISSN. 2011; October – December, 1 (4): 312 – 315.
Dekker G, Sibai B. Primary, Secondary and tertiary prevention of preeclampsia. The lancet 2001; January 20, 357: 209 – 215.
Koopmans CM, Bijlenga D, Groen H, Vijgen SM, Aarnoudse JG. et al. for the HYPITAT study group. Induction of labour versus expectant monitoring for gestational hypertension or mild Preeclampsia after 36 week’s gestation (HYPITAT): A multicentre, Open–label randomized controlled trial. www.thelancet.com online 4 Aug, 2009; DOI: 10. 1016/ So 140 – 6736 (09) 60736 – 4.
Steingrub J.S. Pregnancy associated severe liver dysfunction. Crit. care clin. 2004; 20: 763 – 776.
Hussain H. Study of liver function in severe Preeclampsia and eclampsia. Bangladesh College of physicians and surgeons 2009.
Naib J.M, Siddiqui M.I, Agmal W. Maternal and perinatal outcome in eclampsia, A one year study. J Postgrad med Inst 2004; 18 (3): 470 – 476.
Liu C.M, Cheng P.J, Chang S.D. Maternal complications and perinatal outcomes associated with gestational hypertension and severe preeclampsia in Taiwanese women. J formos med Assoc. 2008; 107 (2): 129 – 138.
Ndaboine E, Kihunrwa A, Rumanyiko R, Beatrice H, Massinde A.N. Maternal and perinatal outcomes among eclamptic patients admitted to Bugando Medical centre, Mwanza Tanzania. African Journal of Reproductive Health March 2012; 16 (1): 35 – 42.
Sultana and Aparna J. Risk factors for preeclampsia and its perinatal outcome. Annals of Biological Research; 2013; 4 (10): 1 – 5.
Kozic J.R, Benton S.J, Hutcheon J.A, Payne B.A, Magee L.A, Dadelszen P.V. Abnormal liver function tests as predictors of adverse maternal outcomes in women with preeclampsia. J obstet gynelcol can 2011; 33 (10): 995 – 1004
Rathi U, Bapat M, Rathi P, Abraham P. Effect of liver disease on maternal and fetal outcome – a prospective study. Indian journal of Gastroenterology 2007; March –April. 26: 59 – 63.
Sibai BM. Diagnosis and management of gestational hypertension and pre-eclampsia.2003; July.102(1)
Boopathi A, kushtagi P. HELLP syndrome in a Government District Hospital on the west coast in south India. International journal of Biomedical research. ISSN 0976-9633 Journal DOI : 10.7439/ ijbr.