Clinical profile and response to tuberculosis treatment in patients with chronic kidney disease
Abstract
Introduction: Tuberculosis (TB) is a major public health problem, especially in the developing countries Patients with CKD have a weakened immune system due to the chronic inflammatory state due to CKD per se, also due to long term renal replacement therapy. Aims of The Study
- To study the clinical profile of tuberculosis in chronic kidney disease patients
- To study the response to anti tubercular treatment including adverse effects.
Methodology: This study was carried out in the Department of Nephrology at Government Stanley Medical College and Hospital, Chennai during the period between October 2018-May 2019. A detailed history was taken, Age, symptomatology, non CKD risk factors like smoking, alcoholism, previous history of pulmonary TB, presence of diabetes mellitus, other infections like HCV, and in case of post-transplant patients, use of induction therapy, any graft dysfunction etc. was noted. The definitions for cure, treatment completed, and treatment failure being used in the study.
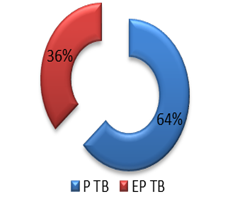
Results: There were a total of 55 patients with CKD diagnosed as tuberculosis by various means-clinical, histopathologic, biochemical, microbiologic, radiologic or a combination of factors.
Conclusion: Tuberculosis is a common infection among Chronic Kidney disease patients, due the immunosuppressed state, hence a high index of suspicion should be maintained, with ways of early screening to be followed based on clinical grounds. Risk factors, namely, smoking, alcoholism, diabetes mellitus predisposes CKD patients to Tuberculosis in addition to the immunosuppressed state of CKD.
Downloads
References
Oxford textbook of tropical medicine p.102
Bentley FJ, Grzybowski S, Benjamin Tuberculosis in Childhood and Adolescence. London: National Association for the Prevention of Tuberculosis, 1954.
Gurbax J. Primary Tuberculosis in Childhood. Springfield, Illinois: CC Thomas,1970.
Miller FJW, Seal RME, Taylor MD et al. Tuberculosis in Children. London: Churchill,1963.
Starke JR, Taylor-Watts KT. Tuberculosis in the pediatric population of Houston, Texas. Pediatrics 1989; 84: 28.
Smith MHD, Marquis JR. Tuberculosis and other mycobacterial infections. In: Feigned, Cherry JD, eds. Textbook of Pediatric Infectious Diseases. Philadelphia: WB Saunders, 1987: 1342.
Pagel W, Simmonds FAH, Macdonald N, Nassau E. Pulmonary Tuberculosis. London: Oxford University Press, 1964.
Proudfoot AT, Akhtar AJ, Douglas AC, Horne NW. Miliary tuberculosis in adults. Br Med J 1969; 2: 273.
Proudfoot AT. Cryptic disseminated tuberculosis. Br J Hosp Med 1971; 5: 773
Ball K, Joules H, Pagel W. Acute tuberculous septicaemia with leucopoenia. Br Med J 1951; ii: 869.
Cooper W. Pancytopoenia associated with disseminated tuberculosis. Ann Intern Med 1959; 50: 1497.
Dawborn JK, Cowling DC. Disseminated tuberculosis and bone marrow dyscrasias. Australas Ann Med 1961; 10: 230.
Hughes JT, John stone RM, Scott AC, Stewart PD. Leukaemoid reactions in disseminated tuberculosis. J Clin Pathol 1959; 12: 307.
Medd WE, Hayhoe FGJ. Tuberculous miliary necrosis with pancytopoenia. Q J Med 1955; 24: 351.
O’Brien JR. Non-reactive tuberculosis. J Clin Pathol 1954; 7: 216.
Oswald NC. Acute tuberculosis and granulocytic disorders. Br Med J 1963; ii: 1489.
Twomey JJ, Leavell BS. Leukemoid reactions to tuberculosis. Arch Intern Med 1965; 116: 21.
Chapman CB, Whorton CM. Acute generalised miliary tuberculosis in adults. A clinico-pathological study based on 63 cases diagnosed at autopsy. N Engl J Med 1946;235: 239.
Lombard EH, Mansvelt EPG. Haematological changes associated with miliary tuberculosis of the bone marrow. Tubercle Lung Dis 1993; 74: 131
Chung DK, Hubbard WW. Hyponatraemia in untreated active pulmonary tuberculosis. Am Rev Respir Dis 1969; 99: 595.