Comparative Study Between Subcuticular Suture and Skin Staples for Skin Closure in Elective Surgery in A Tertiary Care Hospital in Bangladesh
Abstract
Background: With the development of accelerated rehabilitation and the pressure placed on surgeons to reduce length of hospital stay, the method of skin closure has become increasingly important. The ideal surgical wound would be as strong as normal tissue; the moment it is closed. It is widely accepted that both sutures and staples can achieve the basic goals of wound closure. Both methods endeavor to re-approximate the skin by creating a watertight, tension-free, non-inverted opposition of the edges that promotes rapid healing and a cosmetically acceptable scar.
Objective: The aim of the study was to see the comparison between subcuticular suture and skin staples for skin closure in elective surgery.
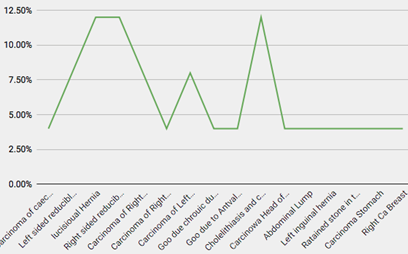
Methods: This prospective type of comparative study was carried out at the department of Surgery, Mugda Medical College and Hospital, Bangladesh, from July 2019 to June 2020. A total of 380 patients were included in this study, divided in two groups based on the technique of wound closure: (i) subcuticular suture and (ii) skin staples group. Data was collected by face-to-face interview using a prepared structured questionnaires & checklist and analyzed on SPSS 22.
Results: Operation time in group I was less than operation time for the same aged group II at 73.55<80.26, which makes suture more efficient. Even the standard deviation error is more prominent in the staple group at 15.53 minutes compared to the suture group at13.65 minutes. The P value is significant at 5% significant level for the Suture group in case of operation time. Comparisons of independent post-operative parameters between two groups of study population. It was observed that majority patients in the poor alignment variable belonged to ‘No’ parameter. The poor alignment of scar variable is significant at 1% significant level. The suture group had lower people belonging in the poor alignment of scar than that of the staple group at 20%<41.58. It can be observed that group II has almost double the samples that have poor alignment of scar than that of the group I. Other post-operative observations, such as the presence of hypertrophic scar and keloid are not significant.
Conclusion: The study suggests that subcuticular suture is comparatively better than skin staples according to BNS score and prospective observation.
Downloads
References
Varghese F, Gamalial J, Kurien JS. Skin stapler versus sutures in abdominal wound closure. Int Surg J. 2017 Sep;4(9):3062-6 [doi: 10.18203/2349-2902.isj20173888].
Sanz L, Smith S. Mechanisms of wound healing, suture material, and wound closure. In: Strategies in gynecologic surgery; 1986. p. 53-76 [doi: 10.1007/978-1-4612-4924-5_5].
Chitrambalam TG, Chandrasekar S, Vinodkumar J, Selva U. Glue versus Staples versus Sutures in Elective Wound Closures: A 3 years Comparative Study. Int J Sci Stud. 2016;4(8):53-6.
Tajirian AL, Goldberg DJ. A review of sutures and other skin closure materials. J Cosmet Laser Ther. 2010 1 Dec;12(6):296-302 [doi: 10.3109/14764172.2010.538413] [Pubmed:21142740].
Reece TB, Maxey TS, Kron IL. A prospectus on tissue adhesives. Am J Surg. 2001 Aug;182(2);Suppl:40S-4S [doi: 10.1016/s0002-9610(01)00742-5] [Pubmed:11566476].
Cirocchi R, Randolph JJ, Montedori A, Cochetti GG, Arezzo A, Mearini EE et al. Staples versus sutures for surgical wound closure in adults. Cochrane Database Syst Rev. 2018 May;2018(5):CD011250.
Lal V, Shaikh TP, Narayan P, Ansari S, Deolekar S. Study of comparison between skin sutures and skin staplers: 400 case studies. Int J Res Med Sci. 2015;3(1):277-81 [doi: 10.5455/2320-6012.ijrms20150150].
Chauhan A, Iqbal M, Singhal A, Niranjan S. Comparative Study of Stapled Skin Closure versus Conventional Skin Closure in Elective Surgeries. JMSCR. 2018;06(06):322-6.
Newman JT, Morgan SJ, Resende GV, Williams AE, Hammerberg EM, Dayton MR. Modality of wound closure after total knee replacement: are staples as safe as sutures? A retrospective study of 181 patients. Patient Saf Surg. 2011 Dec;5(1):26 [doi: 10.1186/1754-9493-5-26] [Pubmed:22011354].
. Bailey and Love’s short practical of surgery. 27th ed. CRC Press; 2018. p. 42 (Williams NS, Ronan P, O’Connell AW. Mccaskie).
Kochar MP, Singh SP. Incised surgical wound closure with sutures and staples. Int Surg J. 2015;2(3):369-72.
Li GQ, Guo FF, Ou Y, Dong GW, Zhou W. Epidemiology and outcomes of surgical site infections following orthopedic surgery. Am J Infect Control. 2013 Dec;41(12):1268-71 [doi: 10.1016/j.ajic.2013.03.305] [Pubmed:23890741].
Edmiston Jr CE, McBain AJ, Roberts C, Leaper D. Clinical and microbiological aspects of biofilm-associated surgical site infections. In: Biofilm-based healthcare-associated infections: I; 2014 9 Oct. p. 47-67.
Owens CD, Stoessel K. Surgical site infections: epidemiology, microbiology and prevention. J Hosp Infect. 2008 Nov;70(2);Suppl 2:3-10 [doi: 10.1016/S0195-6701(08)60017-1] [Pubmed:19022115].
Frishman GN, Schwartz T, Hogan JW. Closure of Pfannenstiel skin incisions. Staples vs. subcuticular suture. J Reprod Med. 1997 Oct;42(10):627-30 [Pubmed:9350017].
Cromi A, Ghezzi F, Gottardi A, Cherubino M, Uccella S, Valdatta L. Cosmetic outcomes of various skin closure methods following cesarean delivery: A randomized trial. Am J Obstet Gynecol. 2010 Jul;203(1):36.e1-8 [doi: 10.1016/j.ajog.2010.02.001] [Pubmed:20417924].
Mackeen AD, Berghella V, Larsen ML. Techniques and materials for skin closure in caesarean section. Cochrane Database Syst Rev. 2012 Sep;11:D3577.
Abdus-Salam RA, Bello FA, Olayemi O. A randomized study comparing skin staples with subcuticular sutures for wound closure at caesarean section in black-skinned women. Int Sch Res Notices. 2014;2014:807937 [doi: 10.1155/2014/807937] [Pubmed:27437457].
Singh B, Mowbray MAS, Nunn G, Mearns S. Closure of hip wound, clips or subcuticular sutures: does it make a difference? Eur J Orthop Surg Traumatol. 2006 Jun;16(2):124-9 [doi: 10.1007/s00590-005-0043-2] [Pubmed:28755123].
Khan RJ, Fick D, Yao F, Tang K, Hurworth M, Nivbrant B, Wood D. A comparison of three methods of wound closure following arthroplasty: a prospective, randomised, controlled trial. J Bone Joint Surg Br. 2006 Feb;88(2):238-42 [doi: 10.1302/0301-620X.88B2.16923] [Pubmed:16434531].
Shetty AA, Kumar VS, Morgan-Hough C, Georgeu GA, James KD, Nicholl JE. Comparing wound complication rates following closure of hip wounds with metallic skin staples or subcuticularvicryl suture: a prospective randomised trial. J Orthop Surg (Hong Kong). 2004 Dec;12(2):191-3 [doi: 10.1177/230949900401200210] [Pubmed:15621905].