Effect of Elective Inguinal Hernia Repair on Urinary Symptoms in Men
Abstract
Background: Urinary symptoms are frequently associated with inguinal hernias and urinary complications occur frequently following repair. Systematic assessment of post-operative urinary symptom burden in patients undergoing elective inguinal hernia repair was not evaluated yet. Therefore, the study was planned to determine the prevalence of urinary symptoms in men undergoing elective inguinal hernia repair.
Methods: This prospective observational study was conducted at the department of surgery in Dhaka Medical College Hospital (DMCH), for 12 months period. Patients with inguinal hernia who were admitted in DMCH were approached and selected in according to the inclusion & exclusion criteria. Before interviewing and before surgical procedure, informed consent was taken from each subject and ethical issues were ensured properly. The researcher did physical examination and assessment of urinary symptoms. Data were collected from a total 100 patients and recorded into a structured questionnaire. Collected data was analyzed by the SPSS 21.
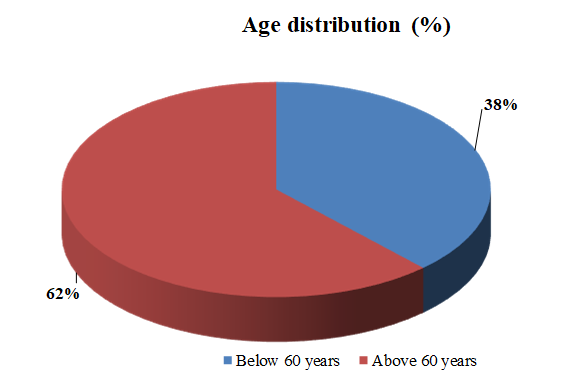
Results: Mean age of the study populations was 60.36 ± 6.87 SD (years) [age range 41-73 years]. About 74% had unilateral inguinal hernia and other 26% had bilateral hernia. Out of 100 patients, 35% patients used perioperative catheter. Only 4% patients had post-operative complications and 2% patients had the history of retention following surgery. The overall median preoperative AUASS score was 6 (range 3 – 28) which increased to 13 (5-33) 48 hours after operation. The increase was statistically significant (p<0.001). The increase in AUASS score noted across all categories of age, BPH, hernia, surgery, anesthesia and surgical technique. During 30 days post-operative follow up, eight patients were lost from follow-up and comparison between preoperative and 30 days post-operative AUASS score showed statistically significant improvement (p<0.001).
Conclusion: Significant improvements of urinary symptoms are seen following elective inguinal hernia repair. However, larger cohort study is needed to finalize the comment.
Downloads
References
Parsons JK, Bergstrom J, Silberstein J, Barrett-Connor E. Prevalence and characteristics of lower urinary tract symptoms in men aged > or =80 years. Urology. 2008; 72:318–321.
Barry MJ. Evaluation of symptoms and quality of life in men with benign prostatic hyperplasia. Urology. 2001; 58:25-32.
Lepor H. Pathophysiology of Benign Prostatic Hyperplasia in the Aging Male Population. Reviews in Urology. 2005;7, S3-S12.
Yalla SV, Sullivan MP, Lecamwasam HS, DuBeau CE, Vickers MA, Carvalho EG Correlation of the American Urological Association symptom index with obstructive and nonobstructive prostatism. J Urol. 1995;153;674-9.
Chancellor MB, Rivas DA. American Urological Association symptom index for women with voiding symptoms: lack of index specificity for benign prostatic hyperplasia. J Urol. 1993;150: 1706-11.
Nitti VW, Kim Y, Combs AJ. Correlation of the AUA symptom index with urodynamics in patients with suspected benign prostatic hyperplasia. Neurourol Urodyn. 1994;13: 521-7.
McVary KT, Roehrborn CG, Avins AL, et al. American Urological Association Guideline: Management of Benign Prostatic Hyperplasia (BPH). Linthicum, MD: American Urological Association; 2010,18-19.
Wagner JP, Brunicardi FC, Amid PK, et al. Schwartz’s Principles of Surgery, Tenth Edition. New York: McGraw-Hill Education. 2015, 1495.
Reis RB, Rodrigues Neto AA, Reis LO, et al. Correlation between the presence of inguinal hernia and the intensity of lower urinary tract symptoms. Acta Cir Bras 2011;26(Suppl 2):125–8
Baldini G, Bagry H, Aprikian A, et al. Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology 2009;110: 1139–57.
Go¨nu¨llu¨ NN, Du¨lger M, Utkan NZ, et al. Prevention of postherniorrhaphy urinary retention with prazosin. Am Surg 1999; 65:55–8.
Darrah DM, Griebling TL, Silverstein JH. Postoperative urinary retention. Anesthesiol Clin 2009;27: 465–84.
Antonescu I, Baldini G, Watson D, et al. Impact of a bladder scan protocol on discharge efficiency within a care pathway for ambulatory inguinal herniorrhaphy. Surg Endosc 2013;27: 4711–20.
Tammela T, Kontturi M, Lukkarinen O. Postoperative urinary retention. II. Micturition problems after the first catheterization. Scand J Urol Nephrol 1986;20: 257–60.
Linares Gil MJ, Esteve Go´mez A, Blanco Vargas D, et al. Factors associated with delayed postsurgical voiding interval in ambulatory spinal anesthesia patients: a prospective cohort study in 3 types of surgery. Am J Surg 2009;197: 182–8.
Ozgu¨n H, Kurt MN, Kurt I, et al. Comparison of local, spinal, and general anaesthesia for inguinal herniorrhaphy. Eur J Surg 2002;168: 455–9.
Jensen P, Mikkelsen T, Kehlet H. Postherniorrhaphy urinary retention– effect of local, regional, and general anesthesia: a review. Reg Anesth Pain Med 2002;27: 612–7.
Kozol RA, Mason K, McGee K. Post-herniorrhaphy urinary retention: a randomized prospective study. J Surg Res 1992;52: 111–2. Petros JG, Rimm EB, Robillard RJ, et al. Factors influencing postoperative urinary retention in patients undergoing elective inguinal herniorrhaphy. Am J Surg 1991;161: 431–3.
Barry MJ, Fowler FJ, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992;148: 1549–57; discussion, 1564.
Reed RD, Poston TL, Kerby JD, Richman JS, Colli JL, Hawn MT. Effect of elective inguinal hernia repair on urinary symptom burden in men. Am J Surg. 2014;208(2):180–6.
Singh S, Prakash R, Singh V, Singh S, Jan SJ. A clinical study of inguinal hernia with special reference to laparoscopic trans-abdominal pre peritoneal repair. Int Surg J. 2017;4(1):282–90.
Mohammadi-Fallah M, Hamedanchi S, Tayyebi-Azar A. Preventive effect of tamsulosin on postoperative urinary retention. Korean J Urol 2012;53: 419–23.
Sentürk AB, Ekici M, Sahiner IT, Tas T, Cakiroglu B. Relationship between lower urinary tract symptoms and inguinal hernia. Arch Ital di Urol e Androl 2016; 2016;88(4):262–5.
Roadman D, Helm M, Goldblatt MI, Kastenmeier A, Kindel TL, Gould JC, et al. Postoperative urinary retention after laparoscopic total extraperitoneal inguinal hernia repair. J Surg Res. 2018; 231:309–15.
Hudak KE, Frelich MJ, Rettenmaier CR, Xiang Q, Wallace JR, Kastenmeier AS, et al. Surgery Duration Predicts Urinary Retention after Inguinal Herniorraphy: A Single Institution Review. Surg Endosc. 2015;29(11):3246–50.