Evaluation of Caesarean Section Rates at Sylhet MAG Osmani Medical College Hospital Using the Robson Ten Group Classification System
Abstract
Background: The rising rates of Cesarean Section (CS) globally, and particularly in Bangladesh, have sparked concerns about the overuse of this surgical intervention, which may lead to adverse maternal and neonatal outcomes. The World Health Organization (WHO) recommends a population-based CS rate of 10-15%; however, the rates in many regions far exceed this threshold.
Objectives: The aim of the study was to evaluate the CS rates at Sylhet MAG Osmani Medical College Hospital (SOMCH) using the Robson Ten Group Classification System (TGCS), to identify the key factors contributing to the high prevalence of CS, and to provide evidence-based recommendations for reducing unnecessary procedures.
Methods: This cross-sectional observational study was conducted at SOMCH during July 2022 to June 2023. All pregnant women admitted for delivery at ≥28 weeks of gestation were included and categorized into ten groups according to the TGCS based on specific obstetric characteristics. Data were collected using a structured questionnaire and extracted from medical records. Descriptive statistics were used to analyze the distribution of women across the Robson groups, group-specific CS rates, and the contribution of each group to the overall CS rate. Statistical analyses of the results were be obtained by using window-based Microsoft Excel and Statistical Packages for Social Sciences (SPSS-24).
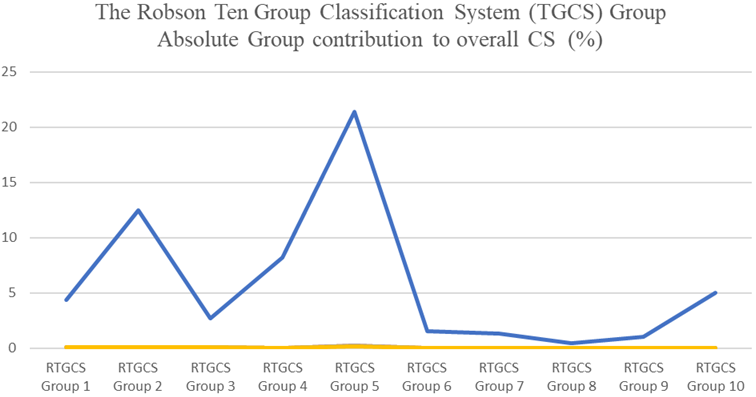
Results: The overall CS rates were reported at Sylhet MAG Osmani Medical College Hospital (SOMCH), 57.43% with 2849 CS cases among 4960 admitted women. The group size, CS rate, and absolute group contribution to overall CS were 24.29%, 36.29%, and 8.81%, respectively in group 1. Another important group includes nulliparous women with single cephalic pregnancies at 37 weeks or more who had induced labor or a CS before labor, which accounted for 11.85% of deliveries with a high CS rate of 72.61% and contributed 8.60% to the overall CS rate. Similarly, multiparous women without a previous CS who received induction or a CS before to labor (Group 4) have a CS rate of 75.83%, accounting for 5.06%.
Conclusion: The study highlights the need for targeted interventions to reduce unnecessary CS procedures at SOMCH. Key recommendations include promoting Vaginal Birth After Cesarean (VBAC), optimizing labor induction practices, and standardizing clinical decision-making processes. Continuous monitoring and evaluation using the TGCS will be essential to ensure that CS is used judiciously, ultimately improving maternal and neonatal health outcomes.
Downloads
References
Abdel-Aleem H, Shaaban OM, Hassanin AI, Ibraheem AA. Analysis of cesarean delivery at Assiut university hospital using the ten-group classification system. International Journal of Gynecology & Obstetrics. 2013 Nov 1;123(2):119-23.
Betrán AP, Torloni MR, Zhang JJ, Gülmezoglu AM, Aleem HA, Althabe F, Bergholt T, De Bernis L, Carroli G, Deneux‐Tharaux C, Devlieger R. WHO statement on caesarean section rates. Bjog. 2016 Apr;123(5):667.
Betran AP, Vindevoghel N, Souza JP, Guelmezoglu AM, Torloni MR. A systematic review of the Robson classification for caesarean section: what works, doesn't work and how to improve it. PloS one. 2014 Jun 3;9(6): e97769.
World Health Organization. Robson classification: implementation manual.
Torloni MR, Betran AP, Souza JP, Widmer M, Allen T, Gulmezoglu M, Merialdi M. Classifications for cesarean section: a systematic review. PloS one. 2011 Jan 20;6(1): e14566.
Calverton M. National Institute of population research and training (NIPORT). Mitra and associate and ORC macro. 2005.
Vogel JP, Betrán AP, Vindevoghel N, Souza JP, Torloni MR, Zhang J, Tunçalp Ö, Mori R, Morisaki N, Ortiz-Panozo E, Hernandez B. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. The Lancet Global Health. 2015 May 1;3(5): e260-70.
WHO H. WHO statement on caesarean section rates. Geneva, Switzerland. 2015 Apr.
Loue VA, Gbary EA, Koffi SV, Koffi AK, Traore M, Konan JK, N’Drin D, Abauleth RY, Kouakou F, Boni SE. Analysis of caesarean rate and indications of university hospitals in sub-Saharan African developing countries using Robson classification system: the case of Cocody’s hospital center, Abidjan-Cote d’Ivoire. Int J Reprod Contracept Obstet Gynecol. 2016 Jun 1;5(6):1773-7.
Kelly S, Sprague A, Fell DB, Murphy P, Aelicks N, Guo Y, Fahey J, Lauzon L, Scott H, Lee L, Kinniburgh B. Examining caesarean section rates in Canada using the Robson classification system. Journal of Obstetrics and Gynaecology Canada. 2013 Mar 1;35(3):206-14.
Robson SJ, De Costa CM. Thirty years of the World Health Organization's target caesarean section rate: time to move on. Medical journal of Australia. 2017 Mar;206(4):181-5.
World Health Organization. Robson classification: implementation manual.
Kelly S, Sprague A, Fell DB, Murphy P, Aelicks N, Guo Y, Fahey J, Lauzon L, Scott H, Lee L, Kinniburgh B. Examining caesarean section rates in Canada using the Robson classification system. Journal of Obstetrics and Gynaecology Canada. 2013 Mar 1;35(3):206-14.
Delbaere I, Cammu H, Martens E, Tency I, Martens G, Temmerman M. Limiting the caesarean section rate in low-risk pregnancies is key to lowering the trend of increased abdominal deliveries: an observational study. BMC pregnancy and childbirth. 2012 Dec; 12:1-0.
Robson M. The Ten Group Classification System (TGCS)-a common starting point for more detailed analysis. BJOG: An International Journal of Obstetrics & Gynaecology. 2015 Apr 1;122(5).
Kibret H, Tadesse B, Debella A, Degefa M, Regassa LD. The Association of Nurses Caring Behavior with the Level of Patient Satisfaction, Harari Region, Eastern Ethiopia. Nursing: Research and Reviews. 2022 Feb; Volume 12:47–56.