Role of Pre-operative Physiotherapy in Reducing Post-operative Complications in Joint Arthroplasty
Abstract
Background: Postoperative complications following total hip and knee arthroplasty remain a significant concern. This study aimed to evaluate the effectiveness of a structured preoperative physiotherapy program in reducing complications and improving outcomes in patients undergoing joint arthroplasty.
Methods: In this randomized controlled trial, 200 patients scheduled for primary total hip or knee arthroplasty were randomly assigned to either a 6-week preoperative physiotherapy program (intervention group, n=100) or standard care (control group, n=100). The primary outcome was the incidence of postoperative complications within 30 days of surgery. Secondary outcomes included length of hospital stay, time to achieve functional milestones, pain scores, and functional outcomes at 3 months post-surgery.
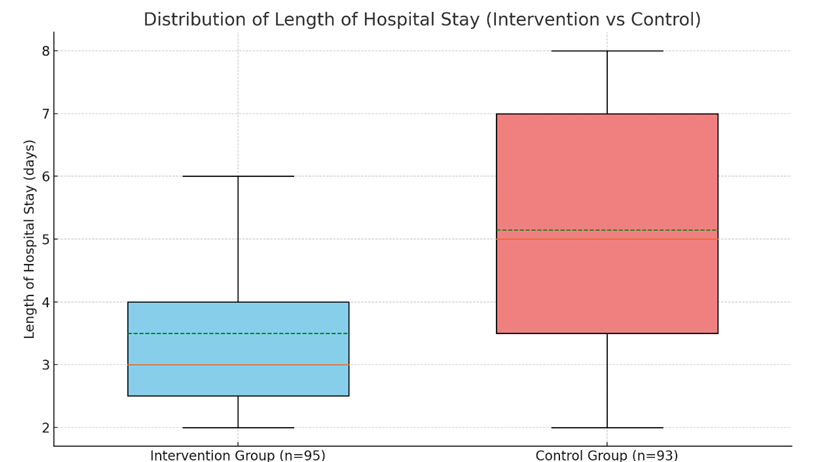
Results: The intervention group demonstrated a significantly lower incidence of postoperative complications compared to the control group (11.6% vs 22.6%, p=0.041). Mean length of hospital stay was shorter in the intervention group (3.2 ± 1.1 days vs 4.1 ± 1.5 days, p<0.001). The intervention group achieved functional milestones earlier, reported lower pain scores, and showed improved functional outcomes at 3 months post-surgery (p<0.05 for all comparisons).
Conclusion: A structured preoperative physiotherapy program significantly reduces postoperative complications and improves functional outcomes in patients undergoing total hip and knee arthroplasty. These findings support the integration of prehabilitation into standard care pathways for joint replacement surgery.
Downloads
References
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-785.
Memtsoudis SG, Pumberger M, Ma Y, et al. Epidemiology and risk factors for perioperative mortality after total hip and knee arthroplasty. J Orthop Res. 2012;30(11):1811-1821.
Wynter-Blyth V, Moorthy K. Prehabilitation: preparing patients for surgery. BMJ. 2017;358:j3702.
Moyer R, Ikert K, Long K, Marsh J. The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: a systematic review and meta-analysis. JBJS Rev. 2017;5(12):e2.
Cabilan CJ, Hines S, Munday J. The effectiveness of prehabilitation or preoperative exercise for surgical patients: a systematic review. JBI Database System Rev Implement Rep. 2015;13(1):146-187.
Hoogeboom TJ, Dronkers JJ, Hulzebos EH, van Meeteren NL. Merits of exercise therapy before and after major surgery. Curr Opin Anaesthesiol. 2014;27(2):161-166.
Gaikwad A, Shigli A, Gupta S, et al. The effect of preoperative physiotherapy in total knee arthroplasty: a systematic review and meta-analysis. J Clin Orthop Trauma. 2020;11(Suppl 5):S868-S878.
Wang L, Lee M, Zhang Z, Moodie J, Cheng D, Martin J. Does preoperative rehabilitation for patients planning to undergo joint replacement surgery improve outcomes? A systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2016;6(2):e009857.
Wallis JA, Taylor NF. Pre-operative interventions (non-surgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery--a systematic review and meta-analysis. Osteoarthritis Cartilage. 2011;19(12):1381-1395.
Gill SD, McBurney H. Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2013;94(1):164-176.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194.
Hoogeboom TJ, Oosting E, Vriezekolk JE, et al. Therapeutic validity and effectiveness of preoperative exercise on functional recovery after joint replacement: a systematic review and meta-analysis. PLoS One. 2012;7(5):e38031.
Peer M, Rush R, Gallacher P, Gleeson N. Pre-surgery exercise and post-operative physical function of people undergoing knee replacement surgery: a systematic review and meta-analysis of randomized controlled trials. J Rehabil Med. 2017;49(4):304-315.
Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248(2):189-198.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205-213.
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737-755.
Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;(248):13-14.
Belmont PJ Jr, Goodman GP, Waterman BR, Bader JO, Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. 2014;96(1):20-26.
Larsen K, Hansen TB, Thomsen PB, Christiansen T, Søballe K. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91(4):761-772.
Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-157.
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57-63.