Comparative Study on Evaluation of Results of DHS/PFN in Management of Intertrochanteric Fracture of Femur
Abstract
Introduction: 38–50% of all femur fractures and 5–20% of fractures in their entirety are intertrochanteric fractures. The prevalence of these fractures is 180/10000, making them prevalent in the senior population. While intramedullary devices like PFN are thought to be superior implants for unstable intertrochanteric fractures, dynamic hip screws are still the gold standard for managing intertrochanteric fractures. Their function in treating these fractures remains questionable.
Materials and Methods: The study was conducted on 100 patients with intertrochanteric fracture of femur attending the outpatient and emergency department of National Institute of Traumatology & Orthopedic Rehabilitation (NITOR), Dhaka between May 2019 to April 2020. Following a clinical and radiological evaluation, the patients were split into two groups at random, A and B. Patients in group A received treatment by ORIF using a dynamic hip screw, whereas patients in group B received treatment via closed/open reduction and internal fixation with PFN. The working proforma below contains the following information of the patient: personal information, clinical findings, radiological findings, and follow-up findings. The outcomes were assessed and contrasted.
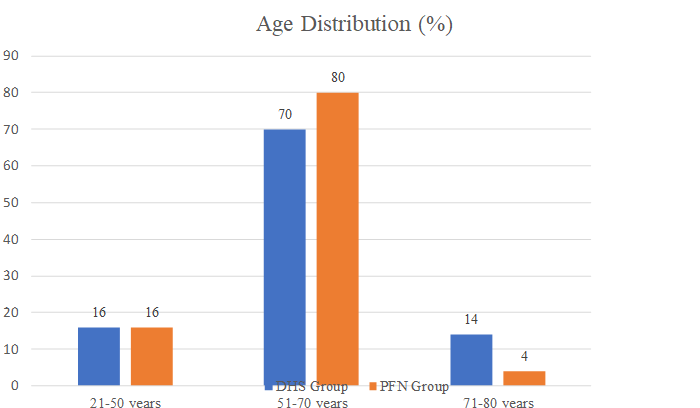
Results: The mean age in both the groups was 58.88 ± 15.76 years, In DHS group, there were 8(16%) females and 42(84%) males. In PFN group, there were 15(30%) females and 35(70%) males. There was a male preponderance in both the groups in comparison to the females. In PFN group, there were 24(48%) patients who injured because of fall, while 26(52%) were injured due to RTA. In PFN group, higher number of fall patients were there, while in DHS group, higher number of RTA patients were there. The comparison of mean blood loss in both the groups showed a statistically significant difference (P < 0.0001), with a higher mean blood loss in DHS group in comparison to PFN group. In DHS group, 48(96%) patients had no complications, 2(4%) had DVT and 1(2%) had cut out of screw, 3(6%) had infection. In PFN group, 2(4%) had infection, 48(96%) shows no complication. The difference in mean union time was significant (P < 0.0001) with a higher union time in DHS group in comparison to PFN group. DHS group functional outcome assessment by Harris Hip score, there were 22(44%) patients had Excellent and the PFN group functional outcome assessment by Harris Hip score, there were 26(52%) patients had Excellent.
Conclusion: PFN provides stability and aids in biological reduction. Excessive collapse and limb shortening are avoided by PFN. As a result, it aids in obtaining a positive functional outcome overall. PFN is a load-bearing implant that provides stability to the fracture area both proximally and distally. As such, it is a more biomechanically sound implant option for fixing peri-trochanteric femoral fractures. When it comes to bleeding during surgery and the early stages of recovery, PFN is a superior implant option than DHS. Consequently, we support the use of PFN rather than DHS in intertrochanteric fractures, with the exception of fractured trochanteric entry points for the PFN.
Downloads
References
2. Felix Bonnaire Æ Henry Zenker Æ Christoph Lill Andreas T. Weber Æ Berend Linke. Treatment strategies for proximal femur fractures in osteoporotic patients Osteoporos Int 2005;16:S93–S102.
3. Marinella MA, Markert RJ. Clinical predictors of prolonged hospitalization in patients with hip fractures. JCOM 2009;16: 453-458.
4. Bentler SE. The aftermath of hip fracture: Amer J Epidemiol 2009;170:1290-1299.
5. Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Inj 2006;37(10):984-989.
6. Craig Lareau, Md, And Gregory Sawyer, Md. Hip Fracture Surgical Treatment and Rehabilitation. Med Health/Rhode Island 2010;93(4).
7. Jože Ferk, Aleksander Frank. Intramedullary nailing of proximal femoral fracture-Postgraduate School Of Surgical Techniques Dhal A, Varghese M, and Bhasin VB: External fixator of intertrochanteric fracture of the femur. JBJS (Br) 1991;73B:955-958.
8. Jewett EL: One-piece angle nail for trochanteric fractures. J Bone Jt Surg 1941;23:803-810.
9. McLoughlin SW, Wheeler DL, Rider J, Bolhofner B: Biomechanical evaluation of the dynamic hip screw with two- and four-hole side plates. J Orthop Trauma 2000;14(5):318-323.
10. W Schumpelick, PM Jantzen: A new principle in the operative treatment of trochanteric fractures of the femur. J Bone Joint Surg 1955.
11. WK Massie et al Fractures of the hip. J Bone Jt Surg Am 1964;1;46(3):658-690.
12. RC Mulholland, DR Gunn - Sliding screw plate fixation of intertrochanteric femoral fractures, The Journal of Trauma and Acute Care Surgery, 1972.
13. William P. Bartels-The Treatment of Intertrochanteric Fractures. J Bone Jt Surg Am 1939;01;21(3):773-775.
14. JE Beltran -Condylo-cephalic nail in pertrochanteric fractures of the neck of the femur. J Bone Jt Surg 1972. Bohler, Collon Treatment of intertrochanteric and subtrochanteric fractures of the hip by the Ender method. J Bone Joint Surg Am 1976;01;58(5):604-611.
15. RT Rosenfeld, DR Schwartz, AH Alter. Leinbach prosthesis in intertrochanteric fractures. J Bone J Surg 1973. 19. Kaufer, Matheull & Sonstegard INJURY: volume 35 issue 10 Oct 2004.
16. Boyd HB and Griffin LL: Classification and treatment of trochanteric fractures. Arch Surg 1949;58:853-866.
17. Wright L. Oblique subcervical (reverse intertrochanteric) fractures of the femur. J Bone J Surg Am 1947;29(3):707- 710.
18. Evans EM: The treatment of trochanteric fractures of the femur. J Bone Jt Surg 1949;31B:190-203. 23. Williams and Parker, 1992. Williams WW, Parker BC: Complications associated with the use of the Gamma nail. Inj 1992;23:291.
19. McConnell T, Tornetta P III, Benson E. Gluteus medius tendon injury during reaming for gamma nail insertion. Clin Orthop 2003;407:199–202.
20. Kyle RF, Gustilo RB and Premer RF: Analysis of six hundred and twenty two intertrochanteric hip fractures. J Bone Jt Surg 1979;61A:216-221.
21. William Townsley. The influence of mechanical factors on the development and structure of bone. 1948;6(1):25–46.
22. Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int 1997;7(5):407-413.
23. GF Stebbing.Fractures of the upper end of the femur. Br J Surg 1927. Hagino H, Furukawa K, Fujiwara S, et al. Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int 2009;20(4):543-548.
24. Mather Cleveland; David M. Bosworth; Frederick R. Thompson; Hudson J. WilsonJR.; Tadao Ishizuka. A TenYear Analysis of Intertrochanteric Fractures of the Femur. J Bone Jt Surg Am 1959;01;41(8):1399-1408.
25. Norton R, Campbell AJ, Lee-Joe T, Robinson E, Butler M. Circumstances of falls resulting in hip fractures among older people. J Am Geriatr Soc 1997;45(9):1108-1112.
26. EB Riska. Prosthetic replacement in the treatment of subcapital fractures of the femur Acta Orthopaedica, 1971.
27. AJ Ingram, B Bachynski. Fractures of The Hip In Children Treatment and Results. J Bone Jt Surg 1953. 34. R Hedlund, U Lindgren. Trauma type, age, and gender as determinants of hip fracture. J orthopaedic res 1987.
28. Kannus P, Parkkari J, Sievanen H, Heinonen A, Vuori I, Jarvinen M.: Epidemiology of hip fractures Bone. 1996;18(1):57S-63S.
29. JC Lotz, EJ Cheal, WC Hayes. Stress distributions within the proximal femur during gait and falls: implications for osteoporotic fracture. Osteoporosis International, 1995.
30. DS Muckle. Iatrogenic factors in femoral neck fractures. Inj 1976.
31. JA Key. Internal fixation of trochanteric fractures of the femur Surgery, 1939.
32. R. C. Murray and J. F. M. Frew, Inverness, Scotland. Trochanteric Fractures of The Femur. J Bone Joint Surg A Plea for Conservative Treatment. From The Orthopaedic Unit, Raigmore Hospital, Inverness 1959.
33. GN Spears, JT Owen.The etiology of trochanteric fractures of the femur. J Bone Jt Surg 1949.
34. Santhosha Jb, Comparative study on evaluation of results of DHS/PFN in management of intertrochanteric fractures femur. J Surg Allied Sci 2019;1(1):17-25