Outcome of Removal of Biliary Stent Prior to Pancreaticoduodenectomy
Abstract
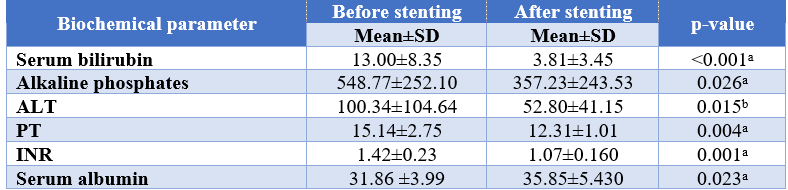
Background: Obstructive jaundice is the commonest manifestation in patients with periampullary carcinoma. Pancreaticodudenctomy is the only curative procedure for resectable tumor. But raised serum bilirubin level may cause the postoperative events. For that reason, preoperative biliary drainage is an important step to reduce the overall postoperative complications. The main aim of this study is to assess the rate of post-operative complications, length of hospital stays and death between patients undergoing pancreaticoduduenectomy with or without removal of biliary stent. Methodology: This prospective cross-sectional study was conducted into department of Surgery and Hepatobiliary, pancreatic and liver transplantation Surgery of BSMMU from July,2017 to June 2018. Initially all the patient diagnosed as periampullary carcinoma and underwent preoperative biliary drainage were enrolled in the study by purposive sampling. Surgery was planned 4-6 weeks after stenting. The analysis was done by student’s t test here. Cross tabulation and chi square test were done to analyze the categorical data. p value was considered as significant at <0.05. Data analysis was done using the software statistical package for social science (SPSS-23. Results: Patients with biliary stent in situ till pancreaticoduodenectomy was significantly associated with positive bile culture (P=0.025) and, E. coli (45.45%) is the most common organism. Post-operative woundinfection was significantly high (p=0.035) in Group A than Group B. From the point of view of postoperative morbidity Group B showed better results than Group A. Microscopic findings of bile duct showed disruption of mucosal epithelium in all 11 (100%) patients in Group A in contrast it was in 3 (33.33%) patients in Group B, which was statistically significant (P value <0.05). Conclusion: Removal of biliary stent before surgery who already underwent preoperative biliary decompression for improvement of liver function showed relatively better outcome after surgery in comparison to those patients in whom pancreaticoduodenectomy was done with keeping stent in situ.
Downloads
References
Hair CD, Sejpal DV (2013). Future developments in biliary stenting. Clin Exp Gastroenterol;6:91–99.
Srinivasan I, Kahaleh M (2011). Biliary stents in the millennium. Adv Ther;28:960–972.
Davids PH, Tanka AK, Rauws EA, van Gulik TM, van Leeuwen DJ, de Wit LT, et al (2003).
Bond-Smith, G., Banga, N., Hammond, T. M., & Imber, C. J. (2012). Pancreatic adenocarcinoma. BMJ, 344, e2476.
Braga, M., Capretti, G., Pecorelli, N., Balzano, G., Doglioni, C., Ariotti, R., et al. (2011). A prognostic score to predict major complications after pancreaticoduodenectomy. Annals of Surgery, 254(5), 702-707.
Karsten TM, Allema JH, Reinders M, Tytgat GN, et al (1996). Preoperative biliary drainage, colonization of bile and postoperative complications in patients with tumors of the pancreatic head: A retrospective analysis of 241 consecutive patients. Eur J Surg; 162:881-888.
Diener, M. K., Fitzmaurice, C., Schwarzer, G., Seiler, C. M., Antes, G., Knaebel, H. P., et al. (2011). Pylorus-preserving pancreaticoduodenectomy (pp whipple) versus pancreaticoduodenectomy (classic whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database of Systematic Reviews (Online), 5, CD006053.
Lindsay J. Jinkins, Abhishek D. Parmar, Yimei Han, Casey B. Duncan, Kristin M. Sheffield, Kimberly M. Brown, and Taylor S. Riall (2013). Current Trends in Preoperative Biliary Stenting in Pancreatic Cancer Patients. Surgery. August ; 154(2): 179–189.
Papadopoulos V, Filippou D, Manolis E, Mimidis K (2007). Haemostasis impairment in patients with obstructive jaundice. J Gastrointestin Liver Dis.;16:177–86.
Sewnath ME, Birjmohun RC, Rauws EA, Huibregste K, Obertop H, Gouma DJ (2001) The effect of preoperative biliary drainage on postoperative complications after pancreaticoduodenectomy. J Am Coll Surg 192:726–734.
van der Gaag NA, Rauws EA, van Eijck CH, Bruno MJ, van der Harst E, Kubben FJ, Gerritsen JJ, Greve JW, Gerhards MF, de Hingh IH, Klinkenbijl JH, Nio CY, de Castro SM, Busch OR, van Gulik TM, Bossuyt PM, Gouma DJ (2010) Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 362:129–137.
Povoski SP, Karpen MS, Conlon KC, et al (1999): Association of preoperative biliary drainage with postoperative outcome following pancreaticoduodenectomy. Ann Surg; 230:131-142.
Khurana, S., Verma, N., Yewdell, J.W., Hilbert, A.K., Castellino, F., Lattanzi, M., Del Giudice, G., Rappuoli, R. and Golding, H., 2011. MF59 adjuvant enhances diversity and affinity of antibody-mediated immune response to pandemic influenza vaccines. Science translational medicine, 3(85), pp.85ra48-85ra48.
Lygidakis, N.J., Van der Heyde, M.N. and Lubbers, M.J., 1987. Evaluation of preoperative biliary drainage in the surgical management of pancreatic head carcinoma. Acta chirurgica scandinavica, 153(11-12), pp.665-668.
Hughes, J.P., Hayashi, I. and Koyama, K., 1998. ASCA X-ray spectroscopy of large magellanic cloud supernova remnants and the metal abundances of the large magellanic cloud. The Astrophysical Journal, 505(2), p.732.
Padillo, J., Puente, J., Gómez, M., Dios, F., Naranjo, A., Vallejo, J.A., Miño, G., Pera, C. and Sitges-Serra, A., 2001. Improved cardiac function in patients with obstructive jaundice after internal biliary drainage: hemodynamic and hormonal assessment. Annals of surgery, 234(5), p.652.
Savader SJ, Trerotola SO, Merine DS, Venbrux AC, Osterman FA. Hemobilia after percutaneous transhepatic biliary drainage: treatment with transcatheter embolotherapy. Journal of Vascular and Interventional Radiology. 1992 May 1;3(2):345-52.
Pers, T.H., Karjalainen, J.M., Chan, Y., Westra, H.J., Wood, A.R., Yang, J., Lui, J.C., Vedantam, S., Gustafsson, S., Esko, T. and Frayling, T., 2015. Biological interpretation of genome-wide association studies using predicted gene functions. Nature communications, 6(1), p.5890.