Neonatal Effects of Thyroid Diseases in Pregnancy and Approach to The Infant With Increased TSH in A Tertiary Care Hospital In Dhaka
Abstract
Background: Thyroid stimulating hormone (TSH) plays a crucial role in embryonic and fetal development from early pregnancy. Both maternal hypothyroidism and hyperthyroidism can significantly impact fetal and neonatal thyroid function, potentially leading to adverse developmental outcomes.
Objective: The aim of this study is to assist pediatricians, neonatologists, and pediatric endocrinologists with the assessment, diagnosis, and treatment of thyroid function disorders and thyroid diseases in the fetus and baby during pregnancy and the neonatal period.
Methods: This prospective cohort study was nested within a larger investigation conducted in Ashiyan Medical College Hospital, Dhaka, Bangladesh.. Pregnant women were recruited between November 2017 and October 2023. Of 1237 invited participants, 266 pregnant women were enrolled, with 4,26 providing blood samples during their first prenatal visit (approximately week 13). Thyroid function was assessed by measuring TSH, free T3 (fT3), and free T4 (fT4) levels across all trimesters.
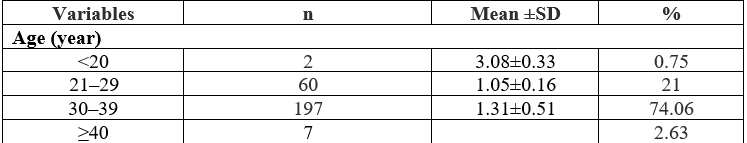
Results: Mean TSH levels showed a progressive increase across trimesters (first: 1.31±0.51 mU/L; second: 1.67±0.77 mU/L; third: 2.36±0.58 mU/L). Child loss was significantly associated with elevated maternal TSH levels, with 41% experiencing miscarriage, 37% fetal death, and 22% neonatal death. The relationship between TSH levels and adverse outcomes persisted even within the normal reference range and after adjusting for confounding factors including parity, smoking, diabetes mellitus, and hypertension.
Conclusions: Elevated maternal TSH levels during pregnancy are associated with increased risk of adverse neonatal outcomes, even in women without overt thyroid dysfunction. These findings suggest that maintaining optimal maternal TSH levels throughout pregnancy is crucial for fetal and neonatal well-being, and support considering treatment for women with even mildly elevated TSH levels. Regular thyroid function monitoring during pregnancy may help identify at-risk cases and improve perinatal outcomes.
Downloads
References
Vulsma T, Gons MH, de Vijlder JJ. Maternal-fetal transfer of thyroxine in congenital hypothyroidism due to a total organification defect or thyroid agenesis. New England Journal of Medicine. 1989 Jul 6;321(1):13-6.
Eng L, Lam L. Thyroid function during the fetal and neonatal periods. Neo Reviews. 2020 Jan 1;21(1): e30-6.
Obregón MJ, Calvo RM, Del Rey FE, De Escobar GM. Ontogenesis of thyroid function and interactions with maternal function. Thyroid gland development and function. 2007; 10:86-98.
SHEPARD TH, Stapp DK. Onset of function in the human fetal thyroid: biochemical and radioautographic studies from organ culture. The Journal of Clinical Endocrinology & Metabolism. 1967 Jul 1;27(7):945-58.
Patel J, Landers K, Li H, Mortimer RH, Richard K. Delivery of maternal thyroid hormones to the fetus. Trends in Endocrinology & Metabolism. 2011 May 1;22(5):164-70.
Korevaar TI, Tiemeier H, Peeters RP. Clinical associations of maternal thyroid function with foetal brain development: Epidemiological interpretation and overview of available evidence. Clinical Endocrinology. 2018 Aug;89(2):129-38.
Fisher DA, Schoen EJ, Franchi SL, Mandel SH, Nelson JC, Carlton EI, Goshi JH. The hypothalamic-pituitary-thyroid negative feedback control axis in children with treated congenital hypothyroidism. The Journal of Clinical Endocrinology & Metabolism. 2000 Aug 1;85(8):2722-7.
Kempers MJ, Van Trotsenburg AS, Van Tijn DA, Bakker E, Wiedijk BM, Endert E, De Vijlder JJ, Vulsma T. Disturbance of the fetal thyroid hormone state has long-term consequences for treatment of thyroidal and central congenital hypothyroidism. The Journal of Clinical Endocrinology & Metabolism. 2005 Jul 1;90(7):4094-100.
Srichomkwun P, Anselmo J, Liao XH, Hönes GS, Moeller LC, Alonso-Sampedro M, Weiss RE, Dumitrescu AM, Refetoff S. Fetal exposure to high maternal thyroid hormone levels causes central resistance to thyroid hormone in adult humans and mice. The Journal of Clinical Endocrinology & Metabolism. 2017 Sep 1;102(9):3234-40.
van der Kaay DC, Wasserman JD, Palmert MR. Management of neonates born to mothers with Graves’ disease. Pediatrics. 2016 Apr 1;137(4).
Daneman D, Howard NJ. Neonatal thyrotoxicosis: intellectual impairment and craniosynostosis in later years. The Journal of pediatrics. 1980 Aug 1;97(2):257-9.
Andersen SL, Laurberg P, Wu CS, Olsen J. Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: a D anish nationwide cohort study. BJOG: An International Journal of Obstetrics & Gynaecology. 2014 Oct;121(11):1365-74.
Casey BM, Thom EA, Peaceman AM and Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Treatment of subclinical hypothyroidism or hypothyroxinemia in pregnancy. N Engl J Med 2017; 376: 815-25.
Bongers-Schokking JJ, Koot HM, Wiersma D, Verkerk PH, de Muinck Keizer-Schrama SM. Influence of timing and dose of thyroid hormone replacement on development in infants with congenital hypothyroidism. J Pediatr 2000; 136: 292–7.
Rovet J, Daneman D. Congenital hypothyroidism: a review of current diagnostic and treatment practices in relation to neuropsychologic outcome. Paediatr Drugs 2003; 5: 141–9.
Grosse SD, Vliet GV. Prevention of intellectual disability through screening for congenital hypothyroidism: how much and at what level? Arch Dis Child 2011; 96: 374–9.
Tillotson SL, Fuggle PW, Smith I, Ades AE, Grant DB. Relation between biochemical severity and intelligence in early treated congenital hypothyroidism: a threshold effect. BMJ 1994; 309: 440–5.
Mutlu M, Karagüzel G, Alıyazicioğlu Y, Eyüpoğlu I, Okten A, Aslan Y. Reference intervals for thyrotropin and thyroid hormones and ultrasonographic thyroid volume during the neonatal period. J Matern Fetal Neonatal Med 2012; 25: 120-4.