Study of Treatment Modalities for Neonatal Pneumothorax in rural tertiary care hospital
Abstract
Introduction: Neonatal pneumothorax, characterized by the accumulation of air in the pleural cavity, is a critical condition observed in up to 9.2% of neonates in neonatal intensive care units (NICUs). It poses risks such as respiratory distress, hemodynamic compromise, intraventricular hemorrhage, and increased mortality. Management strategies include conservative observation, needle aspiration (NA), and intercostal catheter (ICC) insertion, tailored to clinical severity, radiographic findings, and available resources. This study evaluates treatment modalities for neonatal pneumothorax in a rural tertiary care hospital.
Methods: A descriptive longitudinal observational study was conducted from December 2020 to December 2022 at Dr. Balasaheb Vikhe Patil Rural Medical College, Loni. The study included 60 neonates diagnosed with pneumothorax in inborn and outborn NICUs. Exclusion criteria included neonates with major congenital malformations. Data collection encompassed clinical history, diagnostic findings, and management approaches, including observation, CPAP,NA, ICC placement. Statistical analysis evaluated treatment outcomes based on the pneumothorax's side (unilateral or bilateral) and severity.
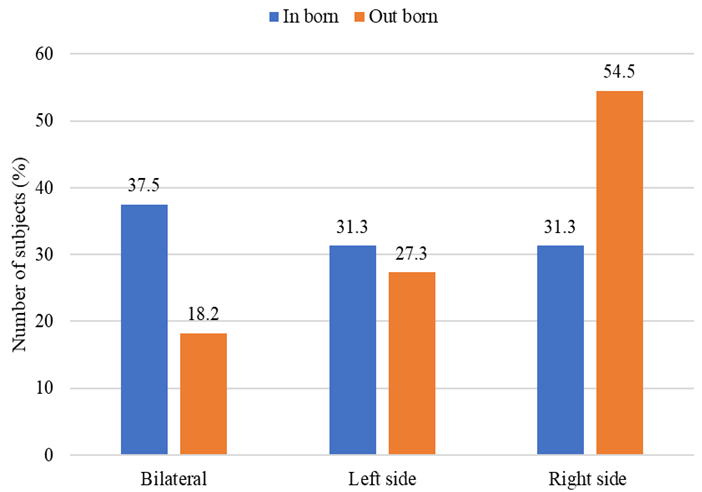
Results: Out of 60 cases, 48.3% had right-sided pneumothorax, 28.3% left-sided, and 23.3% bilateral. CPAP was used in 61.7% of cases, particularly in less severe presentations. Ventilator support was required in 73.3%, with a significantly higher demand among outborn neonates (p=0.03). Needle aspiration was performed in 31.7% of cases, with higher use in left-sided pneumothorax (57%). Chest tube insertion was necessary in 75% of cases, predominantly for right-sided (79.3%) and bilateral pneumothorax (78.5%).
Discussion: The findings align with global studies, highlighting a higher incidence of right-sided pneumothorax due to anatomical predisposition. The study underscores the effectiveness of CPAP in mild cases and the necessity of ICC insertion in severe or bilateral cases. The outcomes advocate for individualized treatment strategies based on clinical severity and resource availability.
Conclusion: Neonatal pneumothorax remains a significant NICU challenge, necessitating prompt diagnosis and tailored interventions. Advances in non-invasive respiratory support and judicious use of mechanical ventilation can mitigate risks. Further research on minimally invasive techniques and long-term outcomes is crucial to optimizing neonatal care and improving survival and neurodevelopmental follow-up.
Downloads
References
Noppen M, De Keukeleire T. Pneumothorax. Respiration 2008;76:121-127
Smith J, Schumacher RE, Donn SM, Sarkar S. Clinical course of symptomatic spontaneous pneumothorax in term and late preterm newborns: report from a large cohort. Am J Perinatol. 2011;28:163–168
Aly H, Massaro A, Acun C, Ozen M. Pneumothorax in the newborn: clinical presentation, risk factors and outcomes. J Matern Fetal Neonatal Med. 2014 ;27:402-406.
Arshad H, Young M, Adurty R, Singh AC. Acute pneumothorax. Crit Care Nurs Q. 2016;39:176–189.
Park SW, Yun BH, Kim KA, SyKo, Lee YK, Shin SM. A Clinical Study abaut Symptomatic Spontaneous pneumothorax. Korean J Perinatol. 2006;17:304–309.
Vibede L, Vibede E, Bendtsen M.· Pedersen L. Ebbesen F. Neonatal Pneumothorax: A Descriptive Regional Danish Study. Neonatology 2017;111:303-308
Ogata ES, Gregory GA, Kitterman JA, et al. Pneumothorax in the respiratory distress syndrome: incidence and effect on vital signs, blood gases, and pH. Pediatrics 1976;58:177–83. 3.
Goldberg RN, Abdenour GE. Air leak syndrome. In: Spitzer AR, ed. Intensive care of the fetus and neonate. St. Louis, MO: Mosby- Yearbook; 1996:629–40.
Horbar JD, Badger GJ, Carpenter JH, et al. Trends in mortality and morbidity for very low birth weight infants, 1991–1999. Pediatrics 2002;110:143–51.
Yu VYH, Liew SW, Roberton NRC. Pneumothorax in the newborn. Arch Dis Child 1975;50:449–53.
Watkinson M, Tiron I. Events before the diagnosis of a pneumothorax in ventilated neonates. Arch Dis Fetal Neonatal Ed 2001;85: F201–3.
Geary C, Caskey M, Fonseca R, Malloy M. Decreased incidence of bronchopulmonary dysplasia after early management changes, including surfactant and nasal continuous positive airway pressure treatment at delivery, lowered oxygen saturation goals, and early amino acid administration: a historical cohort study. Pediatrics 2008;121:89–96.
Jacobsen T, Gronvall J, Petersen S, Andersen GE. ‘‘Minitouch’’ treatment of very low-birth-weight infants. Acta Paediatr 1993;82: 934–8.
Morley CJ, Davis PG, Doyle LW, et al. COIN trial investigators. N Engl J Med 2008;358:700–8.
Stevens TP, Harrington EW, Blennow M, Soll RF. Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants or at risk for respiratory distress syndrome. Cochrane Database Syst Rev 2007; 17:CD003063.
Meberg A, Greve-Isdahl M, Heier CA. Pulmonary air-leakage in newborn infants. Tidsskr Nor Laegeforen 2007;20:2371–3.
Wiswell TE, Tuggle JM, Turner BS. Meconium aspiration syndrome: have we made a difference? Pediatrics 1990;85:715–21.
Ringer SA. Part 3: pneumothorax and air leak. In: Hansen AR, Puder M, editors. 2002 Manual of neonatal surgical intensive care. 2nd ed. Shelton: People’s Medical Publishing House; 2009. p. 188–190.
Ali R, Ahmed S, Qadir M, et al. Pneumothoraces in a neonatal tertiary care unit: case series. Oman Med J. 2013;28(1):67–69.
B APILIOGULLARI, GS SUNAM, S CERAN1 AND H KOC. Evaluation of Neonatal Pneumothorax. The Journal of International Medical Research 2011; 39: 2436 – 2440
Lim HS, Kim H, Jin JY, Shin YL, Park JO, Kim CH, Kim SS. Characteristics of pneumothorax in a neonatal intensive care unit. J Korean Soc Neonatol. 2011 Nov 25;18(2):257-64.
Hany Aly, An Massaro, Ceyda Acun & Maide Ozen (2014) Pneumothorax in the newborn: clinical presentation, risk factors and outcomes, The Journal of Maternal-Fetal & Neonatal Medicine, 27:4, 402-406
Silva IS, Flôr-de-Lima F, Rocha G, Alves I, Guimarães H. Pneumothorax in neonates: a level III Neonatal Intensive Care Unit experience. Journal of Pediatric and Neonatal Individualized Medicine (JPNIM). 2016 Sep 14;5(2):e050220-.
Mannan MA, Dey SK, Jahan N, Iqbal S, Karim SR, Ferdous N. Spectrum of Neonatal Pneumothorax at a Tertiary Care Hospital of Bangladesh: A Retrospective Observational Study. Bangladesh Critical Care Journal. 2019 Mar 27;7(1):12-9.
Avadhesh Joshi, Manish Kumar, Grace Rebekah & Sridhar Santhanam (2022) Etiology, clinical profile and outcome of neonatal pneumothorax in tertiary care center in South India: 13 years’ experience, The Journal of Maternal-Fetal & Neonatal Medicine, 35:3, 520-524
Al-Anbari AJ, Abid JK. Evaluation of Pneumothorax in Neonates in Al Immamian Alkadhomain Medical City. European Journal of Molecular & Clinical Medicine. 2020;7(2):214-9.
Jovandaric, M.Z.; Milenkovic, S.J.; Dotlic, J.; Babovic, I.R.; Jestrovic, Z.; Milosevic, B.; Culjic, M.; Babic, S. Neonatal Pneumothorax Outcome in Preterm and Term Newborns. Medicina 2022, 58, 965.
J. Andersson, A. Magnuson & A. Ohlin (2021): Neonatal pneumothorax: symptoms, signs and timing of onset in the post-surfactant era, The Journal of Maternal-Fetal & Neonatal Medicine, DOI: 10.1080/14767058.2021.1882981
Eun-Ah Kim, MD1,2, Jae-Hun Jung, MD1,2, Sang-Yoon Lee, MD1,2, Sook-Hyun Park, MD, PhD1,2, and Ji Sook Kim, MD, PhD1,2 Neonatal Pneumothorax in Late Preterm and Full-Term Newborns with respiratory Distress: A Single-Center Experience