Prevalence and Pattern of Anemia and Micronutrient Deficiencies in Children with Severe Acute Malnutrition at a Tertiary Care Center: A Cross-sectional Study
Abstract
Background: Severe acute malnutrition (SAM) remains a major health concern in developing countries like India, significantly contributing to pediatric morbidity and mortality. Children with SAM are particularly vulnerable to infections and anemia due to impaired immune response and nutritional deficiencies. This study aimed to assess the prevalence and severity of anemia in children under 60 months diagnosed with SAM.
Method: A cross-sectional study was conducted over 11 months at Pravara Institute of Medical Sciences DU, Loni involving 48 children with SAM. Detailed demographic profiles and medical histories were collected using a predesigned proforma. Anthropometric measurements and laboratory investigations, including hemoglobin, serum iron, ferritin, folate, and vitamin B12 levels, were performed. Anemia was classified based on hemoglobin levels into mild, moderate, and severe categories.
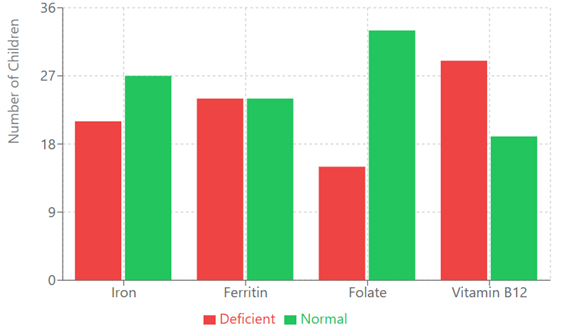
Results: Results revealed that 37 (77.1%) children were anemic, with 9 (24.3%) having mild anemia, 25 (67.6%) moderate anemia, and 3 (8.1%) severe anemia. Low serum iron levels were identified in 21 (43.8%) children, with a higher prevalence in females. Abnormal ferritin levels were observed in 24 (50%), folate deficiency in 15 (31.3%), and vitamin B12 deficiency in 29 (60.4%) children.
Conclusion: Addressing anemia in children with SAM requires early interventions, starting with maternal nutrition during pregnancy and promoting exclusive breastfeeding for the first six months. Continued breastfeeding, appropriate complementary feeding, and caregiver education during routine child health visits are essential. Preventing, detecting, and managing anemia in children with SAM can significantly reduce associated morbidity and mortality.
Downloads
References
Thakur N, Chandra J, Pemde H, Singh V. Anemia in severe acute malnutrition. Nutrition. 2014;30:440-2.
National Family Health Survey (NFHS-3), 2005-06. International Institute for Population Sciences, Mumbai, India. 2007.
National Family Health Survey (NFHS-4), 2015-16. International Institute for Population Sciences, Mumbai, India. 2017.
National Family Health Survey (NFHS-5), 2019-21. International Institute for Population Sciences, Mumbai, India. 2022.
Beniwal N, Chaudhary P, Suman RL. Severe COVID-19 in an infant with severe acute malnutrition. Indian J Pediatr. 2021;88:1158.
WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement. World Health Organization, Geneva, Switzerland. 2009.
Pravana NK, Piryani S, Chaurasiya SP, et al. Determinants of severe acute malnutrition among children under 5 years of age in Nepal: a community-based case-control study. BMJ Open. 2017;7:e017084.
Randev S. Malnutrition in Infants under 6 months: Is it time to change recommendations? Indian J Pediatr. 2020;87:684-5.
Ulahannan SK, Wilson A, Chhetri D, et al. Alarming level of severe acute malnutrition in Indian districts. BMJ Glob Health. 2022;7:e007798.
Chandra J, Kumar P. Anemia in severe acute malnutrition: ten steps of management need to be fine-tuned. Indian J Pediatr. 2023;90:1061-4.
Atiq A, Shah D, Sharma S, et al. Prevalence and predictors of vitamin B12 deficiency in children with severe acute malnutrition, and its association with development. Indian J Pediatr. 2023.
Shukla P, Pandey SK, Singh J, et al. Clinico-etiopathogenesis of vitamin B12, folic acid and iron deficiency in severe acute malnutrition children. Indian J Clin Biochem. 2024;39:221-5.
Yaikhomba T, Poswal L, Goyal S. Assessment of iron, folate and vitamin B12 status in severe acute malnutrition. Indian J Pediatr. 2015;82:511-4.
Sharma SD, Sharma P, Jamwal A, Saini G. Demographic and clinical profile of children with severe acute malnutrition. Int J Sci Study. 2019;7:38-42.
Murthy KA, Malladad A, Kariyappa M. Estimation of serum folate and vitamin B12 levels in children with severe acute malnutrition. Int J Contemp Pediatr. 2020;7:1013-6.
Aggarwal A, Aggarwal A, Goyal S, Aggarwal S. Iron-deficiency anemia among adolescents: a global public health concern. Int J Adv Comm Med. 2020;3:35-40.
Arya AK, Kumar P, Midha T, Singh M. Hematological profile of children with severe acute malnutrition: a tertiary care centre experience. Int J Contemp Pediatr. 2017;4:1577-80.
Chhabra A, Chandar V, Gupta A, Chandra H. Megaloblastic anaemia in hospitalised children. JIACM. 2012;13:195-7.
Kumar R, Singh J, Joshi K, Singh HP, Bijesh S. Co-morbidities in hospitalized children with severe acute malnutrition. Indian Pediatr. 2014;51:125-7.
WHO Guidelines on the Management of Severe Acute Malnutrition in Infants and Young Children. World Health Organization, Geneva, Switzerland. 2013.