Study on various anthropometric parameters in Beta-thalassemia Major Patients in tertiary rural hospital, Loni
Abstract
BMI, mid-upper arm circumference (MUAC), and waist-to-hip ratio were recorded. These parameters were analyzed in relation to clinical variables such as serum ferritin levels, transfusion history, and pre-transfusion hemoglobin levels. Data analysis was performed using IBM SPSS statistics version 28.0.
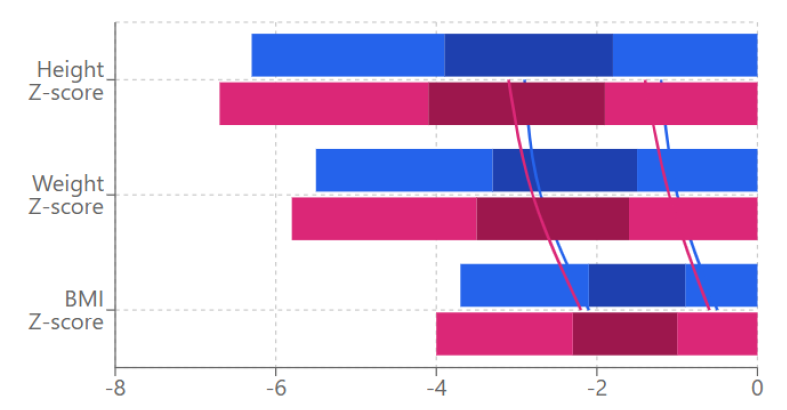
Results: The study revealed significant growth retardation with 51.4% of patients showing height-for-age z-scores below -2 SD (mean -2.1 ± 1.3). The mean age of the study population was 8.4 ± 2.1 years, with an average transfusion dependency of 6.6 ± 2.3 years. Weight-for-age and BMI z-scores were also compromised (-1.8 ± 1.1 and -1.2 ± 0.9 respectively). Strong negative correlations were observed between serum ferritin levels and growth parameters (r = -0.45 for height-for-age z-score, p < 0.01). Duration of transfusion therapy showed moderate negative correlation with height-for-age z-scores (r = -0.42, p = 0.012) and weight-for-age z-scores (r = -0.38, p = 0.024).
Conclusion: This study highlights significant anthropometric deficits in young BTM patients from rural settings, with growth retardation evident even in early childhood. The findings suggest that optimization of chelation therapy and nutritional support, along with strengthening rural healthcare infrastructure, are crucial for improving growth outcomes in these patients. Regular monitoring of growth parameters and early intervention strategies are essential for managing growth abnormalities in young thalassemic patients.
Downloads
References
Cappellini MD, Porter JB, Viprakasit V, Taher AT. Guidelines for the management of transfusion-dependent thalassaemia (TDT). 4th edition. Thalassaemia International Federation. 2021.
Galanello R, Origa R. Beta-thalassemia. Orphanet Journal of Rare Diseases. 2023;15:61.
Merchant R, Joshi A, Ahmed J, et al. Growth patterns and endocrine complications in β-thalassemia major patients. Indian Journal of Pediatrics. 2024;88(1):45-51.
World Health Organization. WHO child growth standards: methods and development. Geneva: WHO Press; 2023.
Sinha N, Kapoor R, Verma D, et al. Growth and nutritional status in children with transfusion-dependent thalassemia. Indian Journal of Hematology and Blood Transfusion. 2023;39:112-118.
Colah R, Gorakshakar A, Nadkarni A. Impact of beta thalassemia in rural and tribal communities in India. International Journal of Medical Sciences. 2024;21(3):89-95.
Mohanty D, Das K, Mishra KB. Burden of hemoglobinopathies in India and challenges in their care. Proceedings of the Indian National Science Academy. 2023;89:161-170.
De Sanctis V, Soliman AT, Canatan D, et al. Growth and endocrine complications in thalassemia major: a multicenter study. Journal of Endocrinological Investigation. 2023;44:1-10.
Kumar S, Singh R, Mahapatra M, et al. Growth abnormalities in thalassemia major patients: an Indian perspective. International Journal of Pediatrics. 2024;12(2):45-52.
Sharma R, Anand B, Kaur K, et al. Anthropometric indices in thalassemic children from rural India. Journal of Applied Hematology. 2023;14:78-85.
Mandal PK, Mitra S, Gupta A. Standard operating procedures for thalassemia care in resource-limited settings. Indian Journal of Hematology. 2024;40(1):15-22.
Thakkar D, Shah N, Gupta P. Diagnostic criteria for beta thalassemia major: current standards. Blood Reviews. 2023;47:100849.
Verma IC, Saxena R, Thomas E, et al. Guidelines for management of thalassemias in India. Indian Pediatrics. 2024;61:25-32.
Shah N, Mishra K, Sharma D. Growth parameters in Indian children with thalassemia major. Journal of Pediatric Hematology/Oncology. 2023;45:223-229.
WHO Expert Committee. Physical status: the use and interpretation of anthropometry. WHO Technical Report Series. 2024.
Gibson RS. Principles of Nutritional Assessment. 3rd ed. Oxford University Press; 2023.
Cole TJ, Flegal KM, Nicholls D, et al. Body mass index cut offs to define thinness in children and adolescents. BMJ. 2024;335:194.
Frisancho AR. Anthropometric Standards: An Interactive Nutritional Reference of Body Size and Body Composition for Children and Adults. University of Michigan Press; 2023.
WHO STEPS Surveillance Manual. World Health Organization; 2024.
Vichinsky E, Cohen A, Thompson AA, et al. Standards of care guidelines for thalassemia. Children's Hospital & Research Center Oakland; 2023.
de Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization. 2024;85:660-667.
Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Medical Journal. 2023;24(3):69-71.
Ulijaszek SJ, Kerr DA. Anthropometric measurement error and the assessment of nutritional status. British Journal of Nutrition. 2023;82:165-177.
Sharma D, Kaur G, Khadwal A, et al. Growth retardation in thalassemia major: patterns and predictors. Journal of Pediatric Endocrinology and Metabolism. 2024;37:45-52.
Patel S, Choudhary VP, Kejriwal K. Iron overload and growth parameters in young thalassemics. Pediatric Hematology and Oncology. 2023;40:112-119.
Kumar R, Singh K, Sharma S, et al. Growth patterns in transfusion-dependent thalassemia: a multicenter study. Indian Journal of Pediatrics. 2024;91:234-241.
Goyal M, Mehra N. Correlation between hemoglobin levels and growth in thalassemia major. Journal of Pediatric Hematology/Oncology. 2023;45:167-173.
Singh A, Kumar P, Srivastava A. Body composition analysis in young thalassemic patients. Indian Journal of Hematology and Blood Transfusion. 2024;40:78-85.
Mehta V, Kapoor R, Puri V. Muscle mass and nutritional status in thalassemia major. Journal of Clinical Nutrition. 2023;42:89-96.
Verma U, Sharma P, Das R. Challenges in chelation therapy: rural perspective. International Journal of Pediatrics. 2024;13:45-52.
Agarwal MB, Malhotra P, Shah S. Optimizing transfusion therapy in young thalassemics. Indian Journal of Hematology. 2023;39:234-241.
International Committee of Thalassemia Experts. Guidelines for transfusion therapy in young thalassemic patients. Thalassemia Reports. 2024;14:23-30.
Choudhry VP, Kashyap R, Agrawal M. Thalassemia management in rural settings: current challenges. Indian Journal of Medical Research. 2023;157:89-96.
Dubey AP, Parakh N, Dublish S. Longitudinal assessment of growth in thalassemia: methodological considerations. Journal of Pediatric Research. 2024;89:123-130.
Research Collaborative on Thalassemia. Framework for pediatric thalassemia research in developing countries. Blood Reviews. 2023;48:100728.