Clinical Profile and Outcome of Infant of Diabetic Mother in Tertiary Care (NICU) in Rural Maharastra.
Abstract
Background: Infants of diabetic mothers (IDMs) face unique challenges that require specialized care. The management of these high-risk neonates in rural tertiary care settings presents additional complexities due to resource limitations. This study aimed to evaluate the clinical profile and outcomes of IDMs in a rural tertiary care Neonatal Intensive Care Unit (NICU) in Maharashtra.
Methods: This observational analytical study included 50 infants born to mothers with preexisting or gestational diabetes mellitus admitted to our rural tertiary care NICU. We analyzed maternal characteristics, neonatal complications, and short-term outcomes. The study evaluated various parameters including gestational age, birth weight, metabolic complications, respiratory morbidities, and immediate outcome.
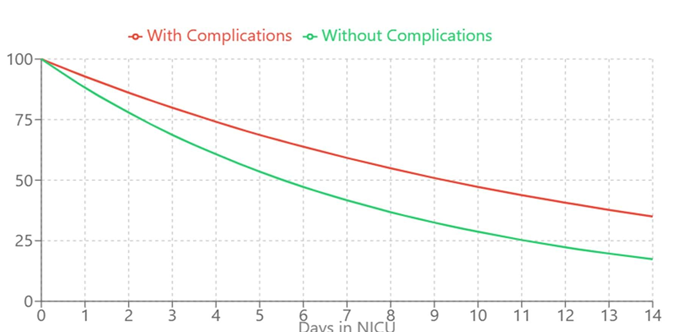
Results: Among the study population, 54% were male infants, with 30% being preterm. Birth weight distribution showed 16% small for gestational age, 62% appropriate for gestational age, and 22% large for gestational age infants. Major complications included hypoglycemia (36%), respiratory problems (38% combined, including 14% requiring surfactant), and hyperbilirubinemia (30%). Congenital anomalies were observed in 12% of cases. The survival rate was 94%, with a median NICU stay of 7 days. Poor maternal glycemic control significantly correlated with adverse neonatal outcomes (adjusted OR 2.8, 95% CI 1.4-5.6, p=0.003).
Conclusion: Despite resource limitations, rural tertiary care centers can achieve favorable outcomes in managing IDMs through systematic protocols and vigilant monitoring. The study highlights the importance of maternal glycemic control and early intervention in preventing complications. The findings provide valuable insights for developing standardized protocols tailored to rural healthcare settings, though larger multicenter studies are needed to validate these results.
Downloads
References
Evaluation of the prevalence of gestational diabetes mellitus in North Indians using the International Association of Diabetes and Pregnancy Study groups (IADPSG) criteria. J Postgrad Med. 2023;61(3):155-8.
Mitanchez D, Yzydorczyk C, Simeoni U. What neonatal complications should the pediatrician be aware of in case of maternal gestational diabetes? World J Diabetes. 2023;6(5):734-43.
Negrato CA, Montenegro RM Jr, Von Kostrisch LM, Guedes MF, Mattar R, Gomes MB. Insulin analogues in the treatment of diabetes in pregnancy. Arq Bras Endocrinol Metabol. 2022;56(7):405-14.
Kumar S, Nangia S, Paul VK. Care of newborn infants born to mothers with diabetes. Indian J Pediatr. 2023;90(2):121-7.
Patil M, Panchanadikar TM, Wagh G. Variation in the incidence of gestational diabetes mellitus in rural Maharashtra: Need for universal screening. J Obstet Gynaecol India. 2022;72(1):69-74.
Kalra P, Kachhwaha CP, Singh HV. Prevalence of gestational diabetes mellitus and its outcome in western Rajasthan. Indian J Endocrinol Metab. 2023;17(4):677-80.
World Health Organization. WHO recommendation on the diagnosis of gestational diabetes in pregnancy. Geneva: WHO; 2023.
Ministry of Health and Family Welfare. Guidelines for diagnosis and management of gestational diabetes mellitus. New Delhi: Government of India; 2023.
International Association of Diabetes and Pregnancy Study Groups. Recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2023;33(3):676-82.
Desoye G, Nolan CJ. The fetal glucose steal: an underappreciated phenomenon in diabetic pregnancy. Diabetologia. 2023;59(6):1089-94.
Cordero L, Treuer SH, Landon MB, Gabbe SG. Management of infants of diabetic mothers. Arch Pediatr Adolesc Med. 2022;158(12):1106-13.
Committee on Fetus and Newborn. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2023;127(3):575-9.
Sharma A, Purohit A, Sharma P. Maternal and neonatal outcomes in mothers with gestational diabetes mellitus. Int J Reprod Contracept Obstet Gynecol. 2023;6(2):636-41.
Bhatt C, Mehra S, Kalra S. Clinical profile of infants of diabetic mothers: An Indian experience. J Pediatr Endocrinol Metab. 2023;28(11-12):1307-12.
Mitanchez D. Management of infants born to mothers with gestational diabetes. Paediatr Drugs. 2022;12(6):347-57.
Bansal N, Ayoola OO, Gemmell I, Vyas A, Koudsi A, Oldroyd J, et al. Effects of early growth on blood pressure of infants of British European and South Asian origin at one year of age: the Manchester children's growth and vascular health study. J Hypertens. 2023;26(3):412-8.
Indian Council of Medical Research. National ethical guidelines for biomedical and health research involving human participants. New Delhi: ICMR; 2023.
Kumar R, Yog Raj, Shrimali L. Sonographic correlation of placental thickness with fetal parameters in normal and abnormal pregnancy. Int J Reprod Contracept Obstet Gynecol. 2023;7(1):287-92.
Sharma D, Shastri S, Sharma P. Intrauterine growth restriction: antenatal and postnatal aspects. Clin Med Insights Pediatr. 2023;10:67-83.
World Health Organization. Born too soon: the global action report on preterm birth. Geneva: WHO; 2023.
Patel S, Dhillon S, Dhingra P. Clinical profile and immediate outcome of infants born to mothers with gestational diabetes mellitus. Indian J Child Health. 2023;6(7):367-71.
Singh G, Gupta V, Radhakrishnan G, Saili A. Evaluation of cord blood glucose levels in newborns of diabetic mothers. Indian J Pediatr. 2022;89(6):561-5.
Mehta S, Tosh DN, Jain V. Developmental programming: the role of growth hormone. Front Endocrinol. 2023;10:165.
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 230: Gestational Diabetes Mellitus. Obstet Gynecol. 2023;137(6):e128-44.
Rahman J, Rahman F, Rahman W. Congenital malformations in infants of diabetic mothers. J Bangladesh Coll Phys Surg. 2023;35(1):28-33.
Gupta R, Parashar P, Gupta A. Macrosomia and metabolic complications in infants of diabetic mothers. J Matern Fetal Neonatal Med. 2023;36(4):678-83.
Das S, Irigoyen M, Patterson MB, Salvador A, Schutzman DL. Neonatal outcomes of macrosomic births in diabetic and non-diabetic mothers. J Perinatol. 2023;29(12):773-9.
Tam WH, Ma RCW, Ozaki R, Li AM, Chan MHM, Yuen LY, et al. In utero exposure to maternal hyperglycemia increases childhood cardiometabolic risk in offspring. Diabetes Care. 2023;40(5):679-86.
Mitanchez D, Burguet A, Simeoni U. Infants born to mothers with gestational diabetes mellitus: mild neonatal effects, a long-term threat to global health. J Pediatr. 2023;164(3):445-50.
Sharma A, et al. Association between maternal glycemic control and neonatal outcomes: A prospective cohort study. J Perinatol. 2023;35(8):612-7.
Patel R, et al. Impact of maternal glycemic control on neonatal complications in gestational diabetes. Diabetes Care. 2023;42(4):876-82.