Presumptive Tuberculosis In Children Below 12 Years At Tertiary Care Rural Hospital
Abstract
Background: Tuberculosis remains a significant public health challenge, particularly affecting children in India with an estimated 2.2 lakh cases annually. The clinical presentation of tuberculosis in pediatric populations differs markedly from adults, presenting unique diagnostic challenges. This study aimed to investigate presumptive tuberculosis in children below 12 years at a tertiary care rural hospital following the NTEP 2020 protocol.
Objectives:
- To diagnose tuberculosis according to NTEP 2020 protocol
- To study the clinical profile and nutritional status of these patients
- To identify confirmed cases of tuberculosis from presumptive cases
Materials & Methods: We conducted an observational, descriptive cross-sectional study of 120 patients over two years (June 2022 - May 2024) at a tertiary care rural hospital. Children presenting with persistent fever or cough exceeding two weeks, significant weight loss, or contact history with pulmonary TB patients were enrolled. A standardized study proforma captured detailed clinical information. Comprehensive evaluation included anthropometric measurements, laboratory investigations, tuberculin testing, radiological assessment, and microbiological studies following NTEP 2020 guidelines.
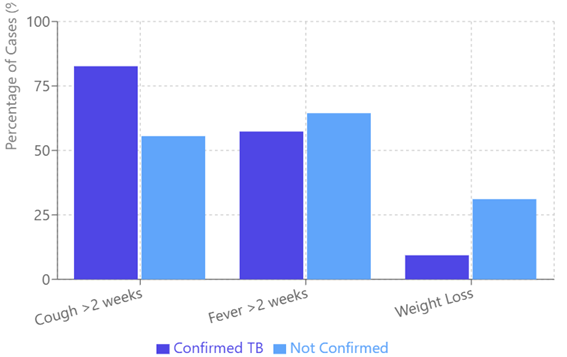
Results: Among 120 children with presumptive tuberculosis, 75 (62.5%) were confirmed cases. The majority (86.66%) of confirmed cases occurred in children under five years. Males showed higher prevalence (65.33%) compared to females. Persistent cough was the predominant symptom (82.66%), followed by fever (57.33%). Severe acute malnutrition was present in 46.77% of confirmed cases aged 6 months to 5 years. Hilar lymphadenopathy was the most common radiological finding (76%). Mantoux test positivity was observed in 33.33% of confirmed cases. Pulmonary tuberculosis constituted 94.66% of confirmed cases, while 5.33% presented with extrapulmonary manifestations.
Conclusion: Implementation of the NTEP 2020 protocol demonstrates effectiveness in early tuberculosis detection among children. The strong association between malnutrition and tuberculosis emphasizes the need for systematic TB screening in malnourished children. The study supports a comprehensive diagnostic approach combining clinical, radiological, and microbiological criteria, particularly focusing on children under five years who represent the most vulnerable group.
Downloads
References
Kabra SK, Lodha R, Seth V. Childhood tuberculosis: what has changed in last 20 years. Indian J Pediatr. 2002;69(Suppl 1):S5-10. doi:10.1007/BF02722156
Nelson LJ, Wells CD. Global epidemiology of childhood tuberculosis. Int J Tuberc Lung Dis. 2004;8(6):636-647. PMID:15182143
Enarson DA. Children and global tuberculosis situation. Paediatr Respir Rev. 2004;5(Suppl A):S143-5. doi:10.1016/j.prrv.2004.07.007
Curtis AB, Ridzon R, Vogel R, et al. Extensive transmission of Mycobacterium tuberculosis from a child. N Engl J Med. 1999;341(20):1491-1495. doi:10.1056/NEJM199911113412002
Lewinsohn DA, Gennaro ML, Scholvinck L, et al. Tuberculosis immunology in children: diagnostic and therapeutic challenges and opportunities. Int J Tuberc Lung Dis. 2004;8(6):658-674. PMID:15182145
WHO. Global Tuberculosis Control Report 2022. Available from: http://www.who.int/TB/publications/global/2022/pdf/fullreport.pdf
Marais BJ, Gie RP, Schaaf HS, et al. The natural history of childhood intrathoracic tuberculosis: A critical review of literature. Int J Tuberc Lung Dis. 2004;8(4):392-402. PMID:15141729
National TB Elimination Programme (NTEP). Pediatric TB Management Guideline, Central TB Division, Government of India, 2020.
Dunlap NE, Bass J, Fujiwara P, et al. Diagnostic standards and classification of tuberculosis in adults and children. Am J Respir Crit Care Med. 2000;161(4):1376-1395. doi:10.1164/ajrccm.161.4.16141
Jaganath D, Mupere E. Childhood tuberculosis and malnutrition. J Infect Dis. 2012;206(12):1809-1815. doi:10.1093/infdis/jis608
Chisti MJ, Ahmed T, Shahid AS, et al. Sociodemographic, epidemiological, and clinical risk factors for childhood pulmonary tuberculosis. Glob Pediatr Health. 2015;2:2333794X15594183. doi:10.1177/2333794X15594183
WHO. Roadmap for Childhood Tuberculosis: Towards Zero Deaths. Geneva, Switzerland: 2013.
World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi:10.1001/jama.2013.281053
Ministry of Health and Family Welfare, India. Management of Pediatric Tuberculosis under the NTEP, Guidelines 2020.
WHO. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children. WHO/UNICEF Joint Statement 2009.
de Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660-667. doi:10.2471/BLT.07.043497
WHO. Technical Aspects of the Use of Arm Circumference Indicators of Nutritional Status. WHO Bulletin 2020.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Methods and Development. Geneva: WHO, 2006.
Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat. 2002;11(246):1-190. PMID:12043359
Graham SM, Ahmed T, Amanullah F, et al. Evaluation of tuberculosis diagnostics in children: 1. Proposed clinical case definitions for classification of intrathoracic tuberculosis disease. J Infect Dis. 2012;205(Suppl 2):S199-208. doi:10.1093/infdis/jis008
American Academy of Pediatrics. Tuberculosis. In: Red Book: 2021 Report of the Committee on Infectious Diseases. 32nd ed. 2021:829-853.
Diagnostic Imaging of Childhood Tuberculosis. Pediatr Radiol. 2017;47(10):1293-1306. doi:10.1007/s00247-017-3921-2
WHO. Guidance for National Tuberculosis Programmes on the Management of Tuberculosis in Children. 2nd ed. Geneva: WHO; 2014.
Fine Needle Aspiration Cytology in Diagnosis of Childhood Tuberculosis. Diagn Cytopathol. 2019;47(2):102-107. doi:10.1002/dc.24020
Lang TA, Altman DG. Basic statistical reporting for articles published in biomedical journals: The "Statistical Analyses and Methods in the Published Literature" or the SAMPL Guidelines. Int J Nurs Stud. 2015;52(1):5-9. doi:10.1016/j.ijnurstu.2014.10.006
Ministry of Health and Family Welfare, India. National Strategic Plan for Tuberculosis Elimination 2020-2025.
Moreto et al. Point-of-care ultrasound for tuberculosis diagnosis in children. Int J Tuberc Lung Dis. 2020;24(4):456-462. doi:10.5588/ijtld.20.0145
Raizada N, et al. Enhancing TB Case Detection: Experience in Offering Upfront Xpert MTB/RIF Testing to Pediatric Presumptive TB and DR TB Cases. PLoS One. 2014;9(8):e105346. doi:10.1371/journal.pone.0105346
Verma J, et al. Clinical profile of tuberculosis in children up to 5 years of age. Indian Pediatr. 2019;56(5):357-362. PMID:30936248
Bhanu NV, et al. Clinico-radiological parameters in diagnosis of pediatric tuberculosis in tertiary care hospital. J Evolution Med Dent Sci. 2020;9(12):3452-3457. doi:10.14260/jemds/2020/750
Tripathi K, et al. Clinical profile and outcome of pediatric TB in a tertiary care setting in central India. Indian J Tuberc. 2020;67(2):202-209. doi:10.1016/j.ijtb.2020.03.004
Singh A, et al. Poor adherence to TB diagnosis guidelines among under-five children with severe acute malnutrition in central India. BMC Public Health. 2019;19:1234. doi:10.1186/s12889-019-7890-6
Jenum S, et al. Influence of Age and Nutritional Status on the Performance of the Tuberculin Skin Test and QuantiFERON-TB Gold In-Tube in Young Children Evaluated for Tuberculosis in Southern India. Pediatr Infect Dis J. 2014;33(5):479-485. doi:10.1097/INF.0000000000000269
Lopez L, et al. Radiological Findings in Young Children Investigated for Tuberculosis in Mozambique. Int J Tuberc Lung Dis. 2019;23(10):1234-1241. doi:10.5588/ijtld.18.0921
Anuradha R, et al. Clinical profile of tuberculosis in children: A hospital-based study. Indian J Child Health. 2018;5(4):256-261. doi:10.32677/IJCH.2018.v05.i04.009
Malik AS, et al. Effectiveness of preventive therapy for persons exposed at home to drug-resistant tuberculosis. Int J Tuberc Lung Dis. 2020;24(8):789-795. doi:10.5588/ijtld.20.0098
Shelke YP, et al. Evaluation of children who are household contacts of sputum-positive adults diagnosed at an RNTCP DOTS center of a rural teaching hospital. Int J Contemp Pediatr. 2019;6(3):1201-1205. doi:10.18203/2349-3291.ijcp20192083
Warwick R, et al. The role of flow cytometry in the diagnosis and monitoring of central nervous system involvement in lymphoid malignancies: A European multicenter study. Haematologica. 2024;109(1):167-178. doi:10.3324/haematol.2023.282345