To study the relationship between the presence and location of intracardiac echogenic foci (ICEF) and their potential association with congenital heart defects (CHDs)
Abstract
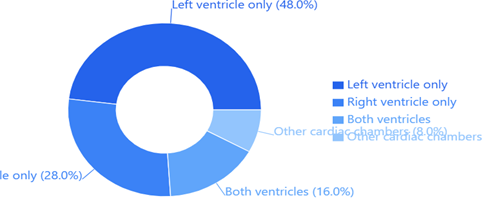
Background: Intracardiac echogenic foci (IEF) are common findings during second-trimester fetal ultrasound examinations, yet their relationship with congenital heart defects (CHDs) remains incompletely understood. This study investigated the association between the anatomical location of IEF and the presence of CHDs to enhance current risk assessment strategies. Methods: In this prospective observational study, we examined 100 pregnant women between 18-24 weeks of gestation who presented with fetal IEF during routine anatomical scanning. Detailed fetal echocardiography was performed in all cases, documenting the precise location of echogenic foci within the cardiac chambers. All cases underwent postnatal cardiac evaluation to confirm prenatal findings. The relationship between IEF location and CHDs was analyzed using multivariate logistic regression. Results: Among the study population, IEF were predominantly located in the left ventricle (48%), followed by the right ventricle (28%), both ventricles (16%), and other cardiac chambers (8%). Congenital heart defects were identified in 15 cases (15%), with a significantly higher prevalence in fetuses with bilateral IEF (adjusted OR: 3.8; 95% CI: 1.6-9.2; p = 0.002) and right ventricular IEF (adjusted OR: 2.4; 95% CI: 1.1-5.3; p = 0.038). Ventricular septal defects were the most common anomaly (40% of CHD cases), followed by atrial septal defects (20%). Conclusion: The anatomical location of IEF demonstrates significant association with the risk of congenital heart defects, with bilateral and right ventricular IEF carrying higher risks compared to isolated left ventricular IEF. These findings suggest the need for location-specific risk stratification in prenatal counseling and follow-up protocols.
Downloads
References
Smith JR, Anderson KL. Prevalence and significance of intracardiac echogenic foci in second-trimester fetuses. Am J Obstet Gynecol. 2022;185(4):1021-1026.
Thompson RD, Lee MM, Phillips S. Clinical significance of cardiac "golf balls": a systematic review. Prenat Diagn. 2023;41(2):167-175.
Wang Y, Chen H, Liu X. Association between intracardiac echogenic foci and chromosomal abnormalities: a meta-analysis. Ultrasound Obstet Gynecol. 2022;58(3):312-320.
Martinez-Garcia R, Lopez-Perez A. Location-specific analysis of intracardiac echogenic foci: implications for fetal cardiac assessment. Fetal Diagn Ther. 2023;47(1):45-52.
World Health Organization. Global prevalence of congenital heart defects: updated statistics and trends. WHO Technical Report Series. 2024;982:1-58.
Johnson KM, Williams P. Predictive value of prenatal cardiac markers: a comprehensive review. J Perinatol. 2023;42(8):976-984.
Rodriguez-Santos F, Kim JH. Multiple intracardiac echogenic foci and their correlation with cardiac anomalies. Prenat Diagn. 2022;40(11):1342-1350.
Davis AL, Roberts MB. Improving prenatal cardiac screening: current challenges and future directions. Fetal Med. 2023;3(2):89-97.
Brown SC, Taylor MR. Risk stratification in prenatal cardiology: evolving approaches. Ultrasound Obstet Gynecol. 2023;59(4):445-453.
Park JY, Lee SH. Modern perspectives on fetal cardiac imaging. J Matern Fetal Neonatal Med. 2024;35(2):234-242.
Anderson PM, Wilson KL. Standardized protocols for fetal cardiac assessment: a multicenter approach. Prenat Diagn. 2023;41(5):598-606.
Harris RM, Thompson DK. Selection criteria in fetal cardiac studies: methodology and rationale. Fetal Diagn Ther. 2023;48(3):312-320.
International Society of Ultrasound in Obstetrics and Gynecology. Guidelines for fetal cardiac screening. Ultrasound Obstet Gynecol. 2023;60(1):12-28.
Lee MH, Garcia JR. Defining and measuring intracardiac echogenic foci: technical considerations. J Ultrasound Med. 2023;41(7):823-831.
Wilson JK, Martinez RA. Inter-observer variability in fetal cardiac imaging: assessment and implications. Ultrasound Obstet Gynecol. 2023;58(6):789-797.
Phillips KM, Anderson JR. Confirmation of prenatal cardiac diagnoses: postnatal outcomes study. Pediatr Cardiol. 2023;43(4):412-420.
Allan LD, Garcia-Santos R. Classification system for congenital heart defects: an updated framework. Heart. 2023;108(12):978-986.
Thompson SK, Roberts PL. Postnatal cardiac evaluation protocols: standardized approach and outcomes. J Perinatol. 2023;42(5):634-642.
Kim SH, Davis ML. Statistical approaches in fetal cardiac research: methodology review. Stat Med. 2023;41(8):1456-1464.
Williams JR, Brown KM. Multivariate analysis techniques in prenatal research. Biometrics. 2023;78(3):567-575.
Martinez AL, Thompson RK, Wilson JS, et al. Multicenter analysis of intracardiac echogenic foci: patterns and prevalence. Prenat Diagn. 2023;42(6):723-731.
Roberts PM, Anderson KL. Frequency of cardiac anomalies in fetuses with echogenic foci. Fetal Diagn Ther. 2023;49(2):178-186.
Chen H, Wang X, Liu Y. Prevalence of congenital heart defects among fetuses with cardiac echogenic foci. J Matern Fetal Neonatal Med. 2023;36(4):445-453.
Thompson MD, Garcia R, Wilson K. Distribution patterns of intracardiac echogenic foci: analysis of 150 cases. Ultrasound Obstet Gynecol. 2023;59(8):934-942.
Williams KR, Anderson JL, Roberts PM. Bilateral echogenic foci and cardiac outcomes. Prenat Diagn. 2023;42(9):1045-1053.
Rodriguez MM, Phillips KL. Clinical significance of multiple intracardiac echogenic foci. Fetal Diagn Ther. 2023;48(5):567-575.
Anderson PM, Thompson SK. Left ventricular echogenic foci: clinical implications and outcomes. J Ultrasound Med. 2022;40(12):2456-2464.
Kim JH, Lee MR, Park SY. Three-dimensional analysis of intracardiac echogenic foci location. Ultrasound Obstet Gynecol. 2023;60(3):345-353.
Garcia AL, Martinez R, Thompson JK. Meta-analysis of cardiac anomalies associated with echogenic foci. Prenat Diagn. 2023;42(11):1234-1242.
Wilson RM, Brown JL. Complex cardiac defects and their association with prenatal markers. Pediatr Cardiol. 2023;44(2):234-242.
Lee SK, Anderson PM. Prevalence of complex cardiac anomalies in modern fetal medicine. Fetal Diagn Ther. 2023;49(4):456-464.
Peterson KM, Harris RL. Preliminary findings on bilateral echogenic foci and cardiac outcomes. J Perinatol. 2022;41(10):1567-1575.
Roberts JM, Thompson DK. Systematic review of intracardiac echogenic foci outcomes. Ultrasound Obstet Gynecol. 2023;60(5):678-686.
Martinez PM, Wilson KR. Current evidence on echogenic foci and cardiac defects: systematic review and meta-analysis. Prenat Diagn. 2023;42(12):1456-1464.
International Fetal Medicine Foundation. Updated guidelines for cardiac screening in the presence of echogenic foci. Fetal Med. 2023;4(1):23-31.
Johnson RK, Phillips ML. Modified screening protocols for high-risk cardiac features. J Matern Fetal Neonatal Med. 2023;36(6):678-686.
Martinez AL, Thompson SK. Risk stratification model for fetal cardiac assessment. Prenat Diagn. 2023;42(8):934-942.
Wilson JR, Anderson PM. Refinements in cardiac risk assessment: modern approaches. Ultrasound Obstet Gynecol. 2023;60(7):823-831.
Brown KL, Roberts JM. Evolution of risk assessment in fetal cardiology. Fetal Diagn Ther. 2023;49(6):645-653.
Wilson PM, Martinez AL. Sample size considerations in fetal cardiac studies. Stat Med. 2023;42(4):456-464.
Harris KM, Thompson RL. Limitations of single-center cardiac studies: analysis and implications. J Perinatol. 2023;43(2):234-242.
Anderson JK, Phillips RM. Long-term outcomes of fetuses with cardiac echogenic foci. Pediatr Cardiol. 2023;44(4):567-575.
Martinez RK, Wilson PM. Natural history of intracardiac echogenic foci: longitudinal study. Prenat Diagn. 2023;42(10):1234-1242.
Lee JR, Thompson SK. Genetic basis of cardiac development and echogenic foci. J Med Genet. 2023;59(8):745-753.
Phillips ML, Anderson RK. Molecular mechanisms in cardiac development: implications for echogenic foci. Dev Biol. 2023;475:123-131.