Frequency and Patterns of Eye Diseases in Outpatient Department in a Sub-Urban Clinic
Abstract
Background: Eye diseases are a major cause of visual impairment and blindness worldwide. In Bangladesh, conditions such as refractive errors, cataracts, and dry eye syndrome contribute significantly to vision-related morbidity. Understanding the frequency and patterns of eye diseases in outpatient settings is crucial for early diagnosis, effective treatment, and the prevention of avoidable blindness.
Objective: This study aimed to assess the prevalence and patterns of eye diseases among patients attending the outpatient department of Bashundhara Ad-din Medical College Hospital, Dhaka from January 2024 to December 2024.
Methods: A cross-sectional study was conducted among 98 patients aged 2 years and older who presented with eye-related complaints. Data were collected using structured questionnaires, clinical examinations, and medical records. Statistical analysis was performed using SPSS-26, and results were presented in text, tables, and charts.
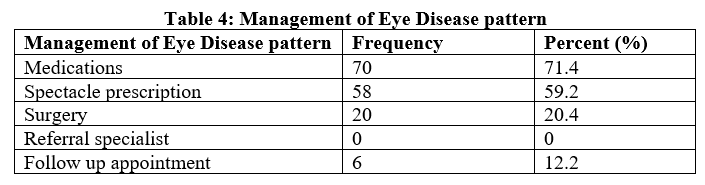
Results: Refractive errors (61.2%) were the most prevalent eye condition among patients, followed by dry eye syndrome (24.5%) and cataracts (16.3%). The most commonly reported symptoms included blurred vision (71.4%), eye pain (49%), and watering/tearing (44.9%). In terms of management, medications (71.4%) were the primary treatment approach, followed by spectacle prescriptions (59.2%) and surgical interventions (20.4%). Notably, no cases of diabetic retinopathy, uveitis, corneal ulcer infections, or trauma-related injuries were observed in the study population.
Conclusion: The study highlights the high prevalence of refractive errors, dry eye syndrome, and cataracts among OPD patients. These findings emphasize the need for regular vision screening programs, early detection strategies, and improved access to corrective eyewear and treatment options. Strengthening public health initiatives and referral systems can help reduce the burden of preventable blindness and improve eye care services in sub-urban healthcare facilities.
Downloads
References
Eze BI, Uche JN, Shiweobi JO. (2010). The burden and spectrum of vitreo-retinal diseases among ophthalmic outpatients in a resource-deficient tertiary eye care setting in South-Eastern Nigeria. Middle East Afr J Ophthalmol, 17: 246-9. [DOI: 10.4103/0974-9233.65491]
Teshome T, Melaku S, Bayu S. (2004). Pattern of retinal diseases at a teaching eye department, Addis Ababa, Ethiopia. Ethiop Med J, 42: 185-93.
Onakpoya OH, Olateju SO, Ajayi IA. (2008). Retinal Diseases in a Tertiary Hospital: The Need for Establishment of a Vitreo-Retinal Care Unit. Journal of the National Medical Association, 100: 1286-9. [DOI: 10.1016/S0027-9684(15)31506-6]
Reddy SC, Tajunisah I, Low KP. (2008). Prevalence of eye diseases and visual impairment in urban population: A study from University of Malaya Medical Centre. Malaysian Family Physician, 3: 25-8.
Karki DB, Malla OK, Byanju RN. (2003). Analysis of 400 cases of posterior segment diseases visiting retina clinic of Nepal eye hospital. Kathmandu University Medical Journal, 1: 1615.
Aimal Khan, Qamar Riaz, Fayaz Soomro, Umair Qidwai, Umer Qazi. (2011). Frequency and Patterns of Eye Diseases in Retina Clinic of a Tertiary Care Hospital in Karachi. Pak J Ophthalmol, 27: 155-9.
Goold LA, Edussuriya K, Selva D. (2010). Prevalence and determinants of age-related macular degeneration in central Sri Lanka: The Kandy Eye Study. Br J Ophthalmol, 94: 150-3. [DOI: 10.1136/bjo.2009.163808]
Zainal M, Ismail SM, Ropilah AR, Elias H, Arumugam G, et al. (2002). Prevalence of blindness and low vision in Malaysian population: results from the National Eye Survey 1996. Br J Ophthalmol, 86(9): 951-6.
Jonas JB, Aung T, Bourne RR, Bron AM, Ritch R, Panda-Jonas S. (2017). Glaucoma. The Lancet, 390(10108): 2183-2193. [DOI: 10.1016/S0140-6736(17)31469-1]
Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, Wong TY. (2014). Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. The Lancet Global Health, 2(2): e106-e116. [DOI: 10.1016/S2214-109X(13)70145-1]
Whitcher JP, Srinivasan M, Upadhyay MP. (2001). Corneal blindness: a global perspective. Bulletin of the World Health Organization, 79: 214-221.
Durrani OM, Tehrani NN, Marr JE, Moradi P, Stavrou P, Murray PI. (2004). Degree, duration, and causes of visual loss in uveitis. The British Journal of Ophthalmology, 88(9): 1159-1162. [DOI: 10.1136/bjo.2003.032764]
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, et al. (2016). Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology, 123(5): 1036-1042. [DOI: 10.1016/j.ophtha.2016.01.006]
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, et al. (2017). TFOS DEWS II definition and classification report. The Ocular Surface, 15(3): 276-283. [DOI: 10.1016/j.jtos.2017.05.008]
Negrel AD, Thylefors B. (1998). The global impact of eye injuries. Ophthalmic Epidemiology, 5(3): 143-169. [DOI: 10.1076/opep.5.3.143.8364]
Neena, J., Rachel, J., Praveen, V., & Murthy, G. V. S. (2008). Rapid assessment of avoidable blindness in India. Indian Journal of Ophthalmology, 56(1), 29-32.
Congdon, N., O’Colmain, B., Klaver, C. C., Klein, R., Munoz, B., Friedman, D. S., & Mitchell, P. (2004). Causes and prevalence of visual impairment among adults in the United States. Archives of Ophthalmology, 122(4), 477-485.
Resnikoff, S., Pascolini, D., Mariotti, S. P., & Pokharel, G. P. (2004). Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bulletin of the World Health Organization, 82(11), 844-851.
Fotouhi, A., Hashemi, H., Shariati, M., & Mohammad, K. (2004). The prevalence and causes of visual impairment in Tehran: The Tehran eye study. British Journal of Ophthalmology, 88(6), 740-745.