Clinical Characteristics and Outcomes of Diabetic Ketoacidosis in School-Age Children: A Single-Center Analysis of 60 Cases
Abstract
Background: Diabetic ketoacidosis (DKA) remains a significant complication in pediatric diabetes, yet specific data focusing on school-age children is limited. This study analyzed the clinical characteristics and outcomes of DKA in this distinct age group to enhance our understanding and improve management strategies.
Methods: We conducted a retrospective analysis of 60 cases of DKA in children aged 6-12 years admitted to our tertiary care center between January 2022 and December 2023. Clinical characteristics, laboratory parameters, treatment outcomes, and complications were evaluated. DKA severity was classified according to venous pH values, and outcomes were analyzed using standardized protocols based on ISPAD guidelines.
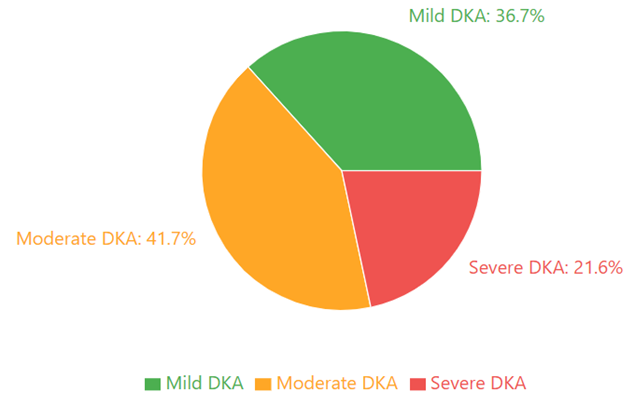
Results: The study included 60 patients (mean age 9.3 ± 2.1 years, 56.7% female), with 31.7% being newly diagnosed cases. DKA severity distribution showed 36.7% mild, 41.7% moderate, and 21.6% severe cases. The median time to DKA resolution was 16.8 hours (IQR: 12.4-22.6), with a mean hospital stay of 3.2 ± 1.4 days. Complications occurred in 13.3% of cases, including cerebral edema (3.3%), hypokalemia (6.7%), and hypoglycemia (3.3%). Among established diabetes cases, insulin omission (46.3%) and technical insulin pump issues (14.6%) were the primary precipitating factors. Multivariate analysis identified severe initial acidosis (pH <7.1) as a significant predictor of prolonged DKA resolution (adjusted OR 2.9, 95% CI 1.3-6.5).
Conclusions: Our findings reveal distinct patterns of DKA presentation and outcomes in school-age children, with notably lower rates of severe cases and complications compared to general pediatric populations. The emergence of insulin pump-related issues as a significant precipitating factor highlights the need for enhanced technical support and education programs. These results support the development of age-specific management protocols and preventive strategies for DKA in school-age children.
Downloads
References
Dabelea D, Rewers A, Stafford JM, et al. Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for diabetes in youth study. Pediatrics. 2014;133(4):e938-45. doi:10.1542/peds.2013-2795
Wolfsdorf JI, Glaser N, Agus M, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr Diabetes. 2018;19(27):155-77. doi:10.1111/pedi.12701
Karges B, Rosenbauer J, Holterhus PM, et al. Hospital admission for diabetic ketoacidosis or severe hypoglycemia in 31,330 young patients with type 1 diabetes. Eur J Endocrinol. 2015;173(3):341-50. doi:10.1530/EJE-15-0129
Cameron FJ, Scratch SE, Nadebaum C, et al. Neurological consequences of diabetic ketoacidosis at initial presentation of type 1 diabetes in a prospective cohort study of children. Diabetes Care. 2014;37(6):1554-62. doi:10.2337/dc13-1904
Kuppermann N, Ghetti S, Schunk JE, et al. Clinical trial of fluid infusion rates for pediatric diabetic ketoacidosis. N Engl J Med. 2018;378(24):2275-87. doi:10.1056/NEJMoa1716816
Dunger DB, Sperling MA, Acerini CL, et al. European Society for Paediatric Endocrinology/Lawson Wilkins Pediatric Endocrine Society consensus statement on diabetic ketoacidosis in children and adolescents. Pediatrics. 2004;113(2):e133-40. doi:10.1542/peds.113.2.e133
Edge JA, Nunney I, Dandi D, et al. Diabetic ketoacidosis in children and adolescents with diabetes. Pediatr Diabetes. 2016;17(S23):65-72. doi:10.1111/pedi.12416
Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D Exchange in 2016-2018. Diabetes Technol Ther. 2019;21(2):66-72. doi:10.1089/dia.2018.0384
Jefferies CA, Nakhla M, Derraik JG, et al. Preventing diabetic ketoacidosis. Pediatr Clin North Am. 2015;62(4):857-71. doi:10.1016/j.pcl.2015.04.002
Rewers A, Klingensmith G, Davis C, et al. Presence of diabetic ketoacidosis at diagnosis of diabetes mellitus in youth: the Search for Diabetes in Youth Study. Pediatrics. 2008;121(5):e1258-66. doi:10.1542/peds.2007-1105
DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;391(10138):2449-62. doi:10.1016/S0140-6736(18)31320-5
Long B, Koyfman A. Emergency medicine evaluation and management of the diabetic ketoacidosis patient. Am J Emerg Med. 2017;35(7):1025-9. doi:10.1016/j.ajem.2017.02.004
Lawrence SE, Cummings EA, Pacaud D, et al. Managing type 1 diabetes in school: Recommendations for policy and practice. Paediatr Child Health. 2015;20(1):35-44. doi:10.1093/pch/20.1.35
Gregory JW, Haines L, Thompson R, et al. British Society for Paediatric Endocrinology and Diabetes guidelines for the management of diabetic ketoacidosis. Arch Dis Child. 2021;106(1):1-9. doi:10.1136/archdischild-2020-319949
Maahs DM, Hermann JM, DuBose SN, et al. Contrasting the clinical care and outcomes of 2,622 children with type 1 diabetes less than 6 years of age in the United States T1D Exchange and German/Austrian DPV registries. Diabetologia. 2014;57(8):1578-85. doi:10.1007/s00125-014-3272-2
Shalitin S, Fisher S, Yackobovitch-Gavan M, et al. Ketoacidosis at onset of type 1 diabetes is a predictor of long-term glycemic control. Pediatr Diabetes. 2018;19(2):320-8. doi:10.1111/pedi.12546
Große J, Hornstein H, Manuwald U, et al. Incidence of diabetic ketoacidosis of new-onset type 1 diabetes in children and adolescents in different countries correlates with human development index (HDI): an updated systematic review, meta-analysis, and meta-regression. Horm Metab Res. 2018;50(3):209-22. doi:10.1055/s-0044-102090
Redel JM, Cherubini V, Liberati AM, et al. Insulin pump therapy in children with type 1 diabetes: analysis of data from the SWEET registry. Pediatr Diabetes. 2018;19(7):1253-61. doi:10.1111/pedi.12755
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-4. doi:10.1001/jama.2013.281053
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344-9. doi:10.1016/j.jclinepi.2007.11.008
Thompson RS, Christie D, Hindmarsh PC, et al. Adherence to insulin pump therapy in adolescents with type 1 diabetes: a systematic review. Diabet Med. 2020;37(7):1077-86. doi:10.1111/dme.14337
Usher-Smith JA, Thompson MJ, Sharp SJ, et al. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ. 2011;343:d4092. doi:10.1136/bmj.d4092
Cherubini V, Grimsmann JM, Åkesson K, et al. Temporal trends in diabetic ketoacidosis at diagnosis of paediatric type 1 diabetes between 2006 and 2016: results from 13 countries in three continents. Diabetologia. 2020;63(8):1530-41. doi:10.1007/s00125-020-05152-1
Wolfsdorf JI, Ratner RE. ISPAD Clinical Practice Consensus Guidelines 2018: Diabetic ketoacidosis in the pediatric patient with type 1 diabetes: an update. Pediatr Diabetes. 2018;19(S27):155-77. doi:10.1111/pedi.12701
Kuppermann N, Ghetti S, Schunk JE, et al. Clinical trial of fluid infusion rates for pediatric diabetic ketoacidosis. N Engl J Med. 2018;378(24):2275-87. doi:10.1056/NEJMoa1716816
Glaser NS, Ghetti S, Casper TC, et al. Pediatric diabetic ketoacidosis, fluid therapy, and cerebral injury: the design of a factorial randomized controlled trial. Pediatr Diabetes. 2013;14(6):435-46. doi:10.1111/pedi.12027
Deeb A, Yousef H, Abdelrahman L, et al. Implementation of a diabetes educator care model to reduce paediatric admission for diabetic ketoacidosis. J Diabetes Res. 2016;2016:3917806. doi:10.1155/2016/3917806
Butalia S, Johnson JA, Ghali WA, et al. Clinical and socio-demographic factors associated with diabetic ketoacidosis hospitalization in adults with Type 1 diabetes. Diabet Med. 2013;30(5):567-73. doi:10.1111/dme.12127
DiMeglio LA, Acerini CL, Codner E, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Glycemic control targets and glucose monitoring for children, adolescents, and young adults with diabetes. Pediatr Diabetes. 2018;19(S27):105-14. doi:10.1111/pedi.12737
Umpierrez GE, Korytkowski M. Diabetic emergencies - ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. Nat Rev Endocrinol. 2016;12(4):222-32. doi:10.1038/nrendo.2016.15
Bialo SR, Agrawal S, Boney CM, et al. Rare complications of pediatric diabetic ketoacidosis. World J Diabetes. 2015;6(1):167-74. doi:10.4239/wjd.v6.i1.167
Glaser N, Barnett P, McCaslin I, et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. N Engl J Med. 2001;344(4):264-9. doi:10.1056/NEJM200101253440404
Glaser NS, Wootton-Gorges SL, Buonocore MH, et al. Frequency of sub-clinical cerebral edema in children with diabetic ketoacidosis. Pediatr Diabetes. 2006;7(2):75-80. doi:10.1111/j.1399-543X.2006.00156.x
Perilli G, Saraceni C, Daniels MN, et al. Diabetic ketoacidosis: a review and update. Curr Emerg Hosp Med Rep. 2013;1(1):10-7. doi:10.1007/s40138-012-0001-3
Desai D, Mehta D, Mathias P, et al. Health care utilization and burden of diabetic ketoacidosis in the U.S. over the past decade: a nationwide analysis. Diabetes Care. 2018;41(8):1631-8. doi:10.2337/dc17-1379
Addala A, Auzanneau M, Miller K, et al. A decade of disparities in diabetes technology use and HbA1c in pediatric type 1 diabetes: a transatlantic comparison. Diabetes Care. 2021;44(1):133-40. doi:10.2337/dc20-0257
Shulman R, Stukel TA, Miller FA, et al. Low socioeconomic status is associated with adverse events in children and teens on insulin pumps under a universal access program: a population-based cohort study. BMJ Open Diabetes Res Care. 2016;4(1):e000239. doi:10.1136/bmjdrc-2016-000239