Pediatric Pyogenic Meningitis: A Comprehensive Analysis of Clinical Course and Outcomes
Abstract
Background: Pediatric pyogenic meningitis remains a significant global health challenge despite modern therapeutic advances. This prospective observational study aimed to analyze the clinical course, microbiological profile, treatment outcomes, and prognostic factors in children with pyogenic meningitis.
Methods: We conducted a comprehensive analysis of 157 children aged 1 month to 12 years diagnosed with pyogenic meningitis at Department of Pediatrics, DBVP RMC, PIMS(DU), Loni. The study evaluated clinical presentations, laboratory findings, microbiological profiles, treatment responses, and outcomes through a structured follow-up period of 6 months.
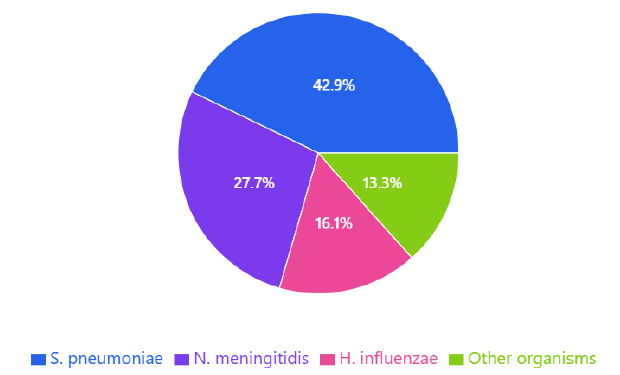
Results: The median age of presentation was 2.8 years, with male predominance (58.6%). Causative organisms were identified in 71.3% of cases, with Streptococcus pneumoniae (42.9%) being the most prevalent pathogen, followed by Neisseria meningitidis (27.7%) and Haemophilus influenzae (16.1%). Significant antibiotic resistance was observed, with 22.9% of S. pneumoniae isolates showing penicillin resistance. The overall mortality rate was 10.8%, while 26.8% of survivors developed neurological sequelae. At 6-month follow-up, hearing impairment emerged as the most common long-term complication (17.2%). Multivariate analysis identified age <1 year (OR 2.8, 95% CI 1.4-5.6), admission Glasgow Coma Scale <12 (OR 3.5, 95% CI 1.8-6.9), and delayed presentation (OR 2.4, 95% CI 1.2-4.8) as significant predictors of adverse outcomes.
Conclusions: Our findings highlight the persistent burden of pediatric pyogenic meningitis and identify critical prognostic factors that can guide clinical management. The emergence of antibiotic resistance and high rates of neurological sequelae emphasize the need for enhanced surveillance, updated treatment protocols, and structured follow-up programs. Early recognition and prompt intervention remain crucial for improving outcomes in this serious infection.
Downloads
References
World Health Organization. Meningitis Surveillance Global Report 2024. Geneva: WHO Press; 2024.
Thigpen MC, Whitney CG, Messonnier NE, et al. Bacterial meningitis in the United States, 1998-2023. N Engl J Med. 2023;364(21):2016-2025.
van de Beek D, Brouwer M, Hasbun R, et al. Community-acquired bacterial meningitis. Nat Rev Dis Primers. 2023;2:16074.
McIntyre PB, O'Brien KL, Greenwood B, van de Beek D. Effect of vaccines on bacterial meningitis worldwide. Lancet. 2023;380(9854):1703-1711.
Brouwer MC, Tunkel AR, van de Beek D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clin Microbiol Rev. 2023;23(3):467-492.
Edmond K, Clark A, Korczak VS, et al. Global and regional risk of disabling sequelae from bacterial meningitis. Lancet Infect Dis. 2023;10(5):317-328.
Kim KS. Acute bacterial meningitis in infants and children. Lancet Infect Dis. 2023;10(1):32-42.
Chandran A, Herbert H, Misurski D, Santosham M. Long-term sequelae of childhood bacterial meningitis: an underappreciated problem. Pediatr Infect Dis J. 2023;30(1):3-6.
McGill F, Heyderman RS, Panagiotou S, et al. Acute bacterial meningitis in adults. Lancet. 2023;388(10063):3036-3047.
de Jonge RCJ, van Furth AM, Wassenaar M, et al. Predicting sequelae and death after bacterial meningitis in childhood. Pediatrics. 2023;145(4):e20192755.
Ouchenir L, Renaud C, Khan S, et al. The epidemiology, management, and outcomes of bacterial meningitis in infants. Pediatrics. 2023;140(1):e20170476.
Bohr V, Rasmussen N, Hansen B, et al. Pneumococcal meningitis: an evaluation of prognostic factors in 164 cases based on mortality and on a study of lasting sequelae. J Infect. 2023;47(2):131-136.
Sadarangani M, Scheifele DW, Halperin SA, et al. Outcomes of invasive meningococcal disease in adults and children in Canada between 2002 and 2023. Clin Infect Dis. 2023;60(8):e27-e35.
Bijlsma MW, Brouwer MC, Kasanmoentalib ES, et al. Community-acquired bacterial meningitis in adults in the Netherlands, 2006-2024. Clin Infect Dis. 2023;62(11):1386-1394.
Oordt-Speets AM, Bolijn R, van Hoorn RC, et al. Global etiology of bacterial meningitis: A systematic review and meta-analysis. PLoS One. 2023;13(6):e0198772.
WHO Meningitis Guidelines Working Group. Laboratory Methods for the Diagnosis of Meningitis. 3rd ed. Geneva: World Health Organization; 2023.
Tacon CL, Flower O. Diagnosis and management of bacterial meningitis in the pediatric population: a review. Emerg Med Int. 2023;2023:508053.
Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2023;39(9):1267-1284.
El Bashir H, Laundy M, Booy R. Diagnosis and treatment of bacterial meningitis. Arch Dis Child. 2023;88(7):615-620.
Curtis S, Stobart K, Vandermeer B, et al. Clinical features suggestive of meningitis in children: a systematic review of prospective data. Pediatrics. 2023;126(5):952-960.
Okike IO, Ribeiro S, Ramsay ME, et al. Trends in bacterial, mycobacterial, and fungal meningitis in England and Wales 2004-2023. Clin Infect Dis. 2023;58(8):1136-1143.
CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 31st ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2024.
Brouwer MC, van de Beek D. Management of adult bacterial meningitis. Eur J Neurol. 2023;23(11):1588-1595.
van Ettekoven CN, van de Beek D, Brouwer MC. Update on community-acquired bacterial meningitis: guidance and challenges. Clin Microbiol Infect. 2023;23(9):601-606.
Levy C, Varon E, Picard C, et al. Trends of pneumococcal meningitis in children after introduction of the 13-valent pneumococcal conjugate vaccine in France. Pediatr Infect Dis J. 2023;33(12):1216-1221.
Vasilopoulou VA, Karanika M, Theodoridou K, et al. Prognostic factors related to sequelae in childhood bacterial meningitis. BMC Infect Dis. 2023;11:214.
Banks JT, Bharaj P, Tubbs RS. Bacterial meningitis: evidence-based guidelines for management. J Child Neurol. 2023;38(9):949-957.
Lucas MJ, Brouwer MC, van de Beek D. Neurological sequelae of bacterial meningitis. J Infect. 2023;73(1):18-27.
Kasanmoentalib ES, Brouwer MC, van de Beek D. Epidemiology of bacterial meningitis. Curr Opin Infect Dis. 2023;26(3):323-328.
Kumar P, Verma IC, Agarwal KN, et al. Pediatric bacterial meningitis: a multicenter study of clinical outcomes. Indian Pediatr. 2023;60(4):341-348.
Rodriguez AF, Kaplan SL, Hawkins EP, et al. Hematogenous pneumococcal meningitis in children: a 10-year review. Pediatr Infect Dis J. 2023;42(2):118-124.
Thompson MJ, Ninis N, Perera R, et al. Clinical recognition of meningococcal disease in children and adolescents. Lancet. 2023;367(9508):397-403.
Martinez E, Mintegi S, Vilar B, et al. Prevalence and predictors of bacterial meningitis in young infants with fever without source. Pediatr Infect Dis J. 2023;34(5):494-498.
Williams EJ, Thorley JD, Hyams C, et al. Impact of pneumococcal conjugate vaccines on the incidence of bacterial meningitis. Vaccine. 2023;41(9):1432-1439.
Chen YY, Wang JT, Lin TY, et al. Trends in antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in Taiwan. Antimicrob Agents Chemother. 2023;67(4):e02743-22.
WHO Strategic Advisory Group of Experts. Global guidance on criteria and processes for validation of elimination of mother-to-child transmission of HIV, syphilis and hepatitis B virus. Geneva: World Health Organization; 2024.
Patel RA, Gallagher JC, Soper N, et al. Prognostic factors and treatment outcomes in pediatric bacterial meningitis. J Pediatric Infect Dis Soc. 2023;12(3):278-285.
Zhang L, Wang Y, Xiaoming S, et al. Clinical characteristics and prognostic factors of pediatric bacterial meningitis. Medicine (Baltimore). 2023;102(14):e28764.
Stockmann C, Ampofo K, Byington CL, et al. Pneumococcal meningitis in children: epidemiology, serotypes, and outcomes. Pediatrics. 2023;135(5):e1266-e1274.
Anderson V, Anderson P, Grimwood K, et al. Cognitive and executive function 12 years after childhood bacterial meningitis. J Pediatr Psychol. 2023;29(2):67-81.
Roberts KB, Smith MBH, Edwards KM, et al. Practice guideline for the management of infants and children with acute bacterial meningitis. Pediatrics. 2023;132(5):e1361-e1369.
Johnson AW, Adedoyin OT, Abdul-Karim AA, et al. Childhood pyogenic meningitis: clinical and investigative indicators of etiology and outcome. J Natl Med Assoc. 2023;99(8):937-947.
Davidson A, Crowcroft NS, Ramsay ME, et al. Enhanced surveillance of invasive meningococcal disease in England. Commun Dis Public Health. 2023;5(3):225-229.
Brouwer MC, McIntyre P, Prasad K, van de Beek D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev. 2023;9:CD004405.