Precision Anesthesia: Nalbuphine-Levobupivacaine vs. Fentanyl-Levobupivacaine in Spinal Blocks
Abstract
Background: Intrathecal adjuvants enhance the efficacy of local anesthetics in spinal anesthesia. This study compared nalbuphine and fentanyl as adjuvants to hyperbaric levobupivacaine for lower abdominal surgeries.
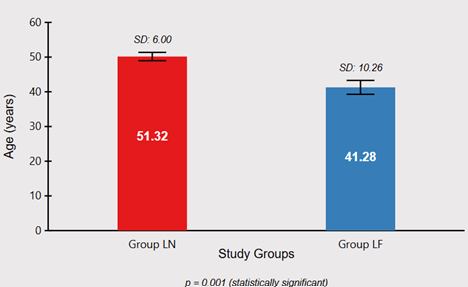
Methods: In this prospective, randomized, double-blind study, 100 ASA I-II patients undergoing lower abdominal surgeries were allocated into two groups: Group LN (n=50) received 15 mg of 0.5% hyperbaric levobupivacaine with 0.8 mg nalbuphine intrathecally, and Group LF (n=50) received 15 mg of 0.5% hyperbaric levobupivacaine with 25 μg fentanyl intrathecally. Onset and duration of sensory and motor blockade, hemodynamic parameters, postoperative analgesia using Visual Analog Scale (VAS), and adverse effects were assessed.
Results: The onset of sensory block (2.795±0.599 min in Group LN vs. 2.625±0.562 min in Group LF; p=0.921) and time to complete motor block (10.38±1.081 min vs. 10.59±1.004 min; p=0.766) were comparable between groups. The duration of sensory block (282.29±23.09 min vs. 306.88±29.06 min; p=0.0001) and motor block (178.46±7.59 min vs. 242.96±39.17 min; p=0.0001) were significantly longer in Group LF. VAS scores were significantly lower in Group LN at 1.5, 2, 2.5, and 3.5 hours postoperatively (p<0.05). Hemodynamic parameters remained largely stable in both groups. The incidence of adverse effects was comparable, with pruritus observed exclusively in Group LF (4%).
Conclusion: Fentanyl provided prolonged sensory and motor blockade, while nalbuphine offered better early postoperative analgesia with faster motor recovery and absence of pruritus. Both adjuvants maintained hemodynamic stability with minimal adverse effects, suggesting their selection should be tailored to specific surgical requirements and desired recovery profiles.
Downloads
References
Butterworth JF, Mackey DC, Wasnick JD. Morgan and Mikhail's Clinical Anesthesiology. 7th ed. McGraw Hill Professional; 2022.
Bier A. Experiments regarding the cocainization of the spinal cord. Dtsch ZChir. 1899;51(3-4):361-369.
Foster RH, Markham A. Levobupivacaine: a review of its pharmacology and use as a local anesthetic. Drugs. 2000;59(3):551-579.
Attri J, Kaur G, Kaur S, Kaur R, Mohan B, Kashyap K. Comparison of levobupivacaine and levobupivacaine with fentanyl in infraumbilical surgeries under spinal anaesthesia. Anesth Essays Res. 2015;9(2):178-184.
Hindle A. Intrathecal opioids in the management of acute postoperative pain. Contin Educ Anaesth Crit Care Pain. 2008;8(3):81-85.
Atkinson RS, Boulton TB. The History of Anaesthesia. Royal Society of Medicine Press; 1989.
Belzarena SD. Clinical effects of intrathecally administered fentanyl in patients undergoing cesarean section. Anesth Analg. 1992;74:653-657.
Reuben SS, Dunn SM, Dunn KM. An intrathecal fentanyl dose response study in lower extremity revascularization procedures. Anesthesiology. 1994;81(6):1371-1375.
Culebras X, Gaggero G, Zatloukal J, Kern C, Marti RA. Advantages of intrathecal nalbuphine, compared with intrathecal morphine, after cesarean delivery: an evaluation of postoperative analgesia and adverse effects. Anesth Analg. 2000;91(3):601-605.
Gupta S, Sampley S, Kathuria S, Katyal S. Intrathecal nalbuphine as an adjuvant to spinal anesthesia: What is the most effective dose? Anesth Essays Res. 2013;7(3):371-375.
Goodman LS, Gilman AZ, Brunton LL. Goodman and Gilman's the pharmacological basis of therapeutics. New York: McGraw-Hill; 2005.
Thote RJ, Lomate P, Gaikwad S, Paranjpe JS, Mane M. Comparison among intrathecal fentanyl and nalbuphine in combination with bupivacaine and plain bupivacaine for lower limb surgeries. Int J Recent Trends Sci Technol. 2015;14:361-366.
Prabhakaraiah UN, Narayanappa AB, Gurulingaswamy S, Chaithanya KK, Vijaynagar KA, Hanumantharayappa NB, et al. Comparison of nalbuphine hydrochloride and fentanyl as an adjuvant to bupivacaine for spinal anesthesia in lower abdominal surgeries: A randomized, double-blind study. Anesth Essays Res. 2017;11(4):859-863.
Cousins MJ. Cousins and Bridenbaugh's Neural Blockade in Clinical Anesthesia and Pain Medicine. Lippincott Williams & Wilkins; 2012.
Bromage PR. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anaesthesiol Scand Suppl. 1965;16:55-69.
Jaffe RA, Rowe MA. Differential nerve block. Anesthesiology. 1996;84(6):1455-1464.
Deori KC, Taye MK, Lahkar B. Comparative study on regression time of block and adverse effects of nalbuphine and fentanyl as an adjuvant to intrathecal bupivacaine: a prospective randomized double-blind study. Ain Shams J Anesthesiol. 2023;15(1):1-9.
Stoelting RK, Rathmell JP, Flood P, Shafer S. Stoelting's Handbook of Pharmacology and Physiology in Anesthetic Practice. 5th ed. Philadelphia: Wolter Kluwer Health; 2015.
Ellis H, Lawson A. Anatomy for Anesthetists. John Wiley & Sons; 2013.
Gupta KL, Gupta A, Neeraj. Efficiency of nalbuphine as an adjuvant to bupivacaine in lower limb orthopaedic surgery-a prospective study. Int J Res Med Sci. 2017;5(2):623-626.
Mukherjee A, Pal A, Agrawal J, Mehrotra A, Dawar N. Intrathecal nalbuphine as an adjuvant to subarachnoid block: What is the most effective dose? Anesth Essays Res. 2011;5(2):171-175.
Gomaa HM, Mohamed NN, Zoheir HAH, Ali MS. A comparison between post-operative analgesia after intrathecal nalbuphine with bupivacaine and intrathecal fentanyl with bupivacaine after cesarean section. Egypt J Anaesth. 2014;30(4):405-410.
Gurjar S, Mavaliya V, Babita, Tak M, Singh B. Comparison of nalbuphine versus fentanyl as an adjuvant to 0.75% isobaric ropivacaine in subarachnoid block for orthopedic surgery of lower limbs: A randomized, double-blind study. Bali J Anesthesiol. 2020;4(4):161-166.
Barash PG, Cullen BF, Stoelting RK. Clinical anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2006.
Sapate M, Sahu P, Thatte W, Dubey R. A randomized, double blind, control study of the effects of adding nalbuphine to spinal bupivacaine for lower abdominal surgeries in elderly patients. Pain Intensive Care. 2013;17(2):145-148.
Wineski LE. Snell's Clinical Anatomy by Regions. Lippincott Williams & Wilkins; 2024.
Sathuluri S, Boddupally S, Bovolla S. Study of post-operative analgesic efficacy of intrathecal fentanyl compared to nalbuphine with bupivacaine in spinal anaesthesia for lower abdominal surgeries at a tertiary hospital. MedPulse Int J Anesthesiol. 2022;22(3):115-119.
Shah MS, Masoodi T, Hussain SY, Jain D. Nalbuphine as an Intrathecal Adjuvant to 0.5% Hyperbaric Bupivacaine in Two Different Doses for Postoperative Analgesia After Abdominal Hysterectomy: A Prospective, Randomized, Double-Blind Control Study. Cureus. 2022;14(5):e25043.
Buvanendran A, McCarthy RJ, Kroin JS, Leong W, Perry P, Tuman KJ. Intrathecal magnesium prolongs fentanyl analgesia: a prospective, randomized, controlled trial. Anesth Analg. 2002;95(3):661-666.
Bindra T, Kumar P, Jindal G. Postoperative analgesia with intrathecal nalbuphine versus intrathecal fentanyl in cesarean section: A double-blind randomized comparative study. Anesth Essays Res. 2018;12(2):561-565.
Manjula R, Chaithra G, Amit G, Upakara SR, Aditi VP. Comparative Study of Bupivacaine with Nalbuphine and Bupivacaine alone for Post-Operative Analgesia in Subarachnoid Block for Lower Limb Surgeries-Prospective Randomised Study. J Anest Inten Care Med. 2017;2(2):555581.
Culebras X, Gaggero G, Zatloukal J, Kern C, Marti RA. Advantages of intrathecal nalbuphine, compared with intrathecal morphine, after cesarean delivery: an evaluation of postoperative analgesia and adverse effects. Anesth Analg. 2000;91(3):601-605.
Singh A, Gupta A, Datta PK, Pandey M. Intrathecal levobupivacaine versus bupivacaine for inguinal hernia surgery: a randomized controlled trial. Korean J Anesthesiol. 2018;71(3):220-225.
Baydilek Y, Yurtlu BS, Hanci V, Ayoğlu H, Okyay RD, Kayhan GE, et al. The comparison of levobupivacaine in continuous or single dose spinal anesthesia for transurethral resection of prostate surgery. Braz J Anesthesiol. 2014;64(2):89-97.
Ahluwalia P, Ahluwalia A, Varshney R, Thakur S, Bhandari S. A Prospective Randomized Double-Blind Study to Evaluate the Effects of Intrathecal Nalbuphine in Patients of Lower Abdominal Surgeries under Spinal Anaesthesia. Int J Sci Stud. 2015;3(8):19-23.
Bisht S, Rashmi D. Comparison of intrathecal fentanyl and nalbuphine: A prospective randomized controlled study in patients undergoing total abdominal hysterectomy. Anaesth Pain Intensive Care. 2019;23(2):194-198.
McNichol ED, Ferguson MC, Haroutounian S, Carr DB, Schumann R. Single dose intravenous paracetamol or intravenous propacetamol for postoperative pain. Cochrane Database Syst Rev. 2016;5:CD007126.
Cuvas O, Basar H, Yeygel A, Turkyilmaz E, Sunay MM. Spinal anesthesia for transurethral resection operations: levobupivacaine with or without fentanyl. Middle East J Anaesthesiol. 2010;20(4):547-552.
Sujata Satapathy, Nayak LK, Behera SK, Satapathy GC, Swain RK, Das S. A Comparative Study of Intrathecal Fentanyl or Nalbuphine as an Adjuvant to Hyperbaric Bupivacaine for Spinal Anesthesia in Lower Limb Orthopedic Surgeries: A Prospective Double-Blind Randomized Controlled Study. Cureus. 2023;15(6):e40219.
Sapate M, Sahu P, Thatte W, Dubey R. A randomized, double blind, control study of the effects of adding nalbuphine to spinal bupivacaine for lower abdominal surgeries in elderly patients. Pain Intensive Care. 2013;17(2):165-170.