Comparison of Outcome Between Anti-Tubercular Therapy Alone and Selective Neck Dissection Followed by Anti-Tubercular Therapy in Retreatment Cases of Tubercular Cervical Lymphadenopathy
Abstract
Background: Tubercular cervical lymphadenopathy (TCL) is a common form of extrapulmonary tuberculosis (EPTB), frequently presenting with painless cervical lymph node swelling. Treatment primarily involves anti-tubercular therapy (ATT), but in cases of relapse or treatment failure, the addition of surgical intervention may enhance outcomes. This study aims to compare the outcomes of ATT alone versus a combination of selective neck dissection (SND) followed by ATT in retreatment cases of tubercular cervical lymphadenopathy.
Methods: A single-blind, randomized controlled trial was conducted at Dhaka Medical College Hospital from January 2022 to July 2023. A total of 48 patients with retreatment cases of TCL were randomly assigned to either Group A (SND + ATT) or Group B (ATT alone). Data were collected on demographic characteristics, clinical presentation, lymph node involvement, diagnostic methods, and treatment outcomes. Patients were followed up every two months for six months to assess treatment efficacy.
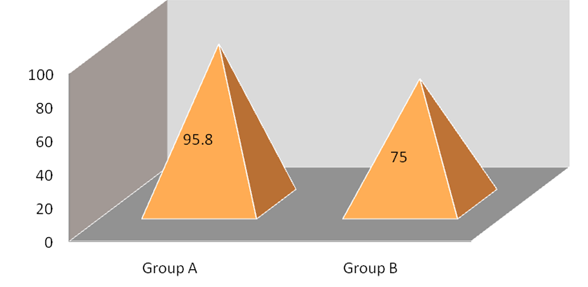
Results: The study found no significant differences in demographic characteristics between the groups. In terms of treatment outcomes, Group A showed a significantly higher cure rate (95.83%) compared to Group B (75.0%) (p = 0.043). Recurrence of disease was significantly lower in Group A (4.16%) than in Group B (25.0%) (p = 0.042). Complication rates were similar between the groups (Group A: 4.16%, Group B: 12.5%), with no significant difference (p = 0.300).
Conclusion: The addition of Selective Neck Dissection to Anti-Tubercular Therapy in retreatment cases of tubercular cervical lymphadenopathy significantly improves cure rates and reduces recurrence without increasing complications. These findings suggest that surgical intervention may be beneficial for patients with TCL who fail or relapse with medical therapy alone.
Downloads
References
World Health Organization. WHO consolidated guidelines on tuberculosis. Module 4: treatment. Tuberculosis care and support. Geneva: World Health Organization; 2022 Apr 30.
Asaduzzaman AKM, Uddin MK, Azad MA, Safi A, Haque WS. Evaluation of Tubercular Cervical Lymphadenopathy: Diagnostic and Therapeutic Utility. Bangladesh J Otorhinolaryngol. 2017;23(2):127-32.
Mohapatra PR, Janmeja AK. Tuberculous lymphadenitis. J Assoc Physicians India. 2009;57(6):585-90.
Fontanilla JM, Barnes A, Von Reyn CF. Current diagnosis and management of peripheral tuberculous lymphadenitis. Clin Infect Dis. 2011;53(6):555-62.
Gautam H, Agrawal SK, Verma SK, Singh UB. Cervical tuberculous lymphadenitis: Clinical profile and diagnostic modalities. Int J Mycobacteriol. 2018;7(3):212-6.
Geldmacher H, Taube C, Kroeger C, Magnussen H, Kirsten DK. Assessment of lymph node tuberculosis in northern Germany: a clinical review. Chest. 2002;121(4):1177-82.
Polesky A, Grove W, Bhatia G. Peripheral tuberculous lymphadenitis: epidemiology, diagnosis, treatment, and outcome. Medicine. 2005;84(6):350-62.
Park KH, Cho OH, Chong YP, Lee SO, Choi SH, Jeong JY, Kim MN, Kim YS, Woo JH, Kim SH. Post-therapy paradoxical response in immunocompetent patients with lymph node tuberculosis. J Infect. 2010;61(5):430-4.
Directorate General of Health Services (DGHS). National Guidelines and Operational Manual for Tuberculosis Control, Fourth Edition. National Tuberculosis Control Programme, Ministry of Health and Family Welfare, Dhaka, Bangladesh; 2021:1-45.
Mukhida S, Vyawahare CR, Mirza SB, Gandham NR, Khan S, Kannuri S, Bhaumi S. Role of GeneXpert MTB/RIF assay for the diagnosis of cervical lymph node tuberculosis and rifampicin resistance. Tzu Chi Med J. 2022;34(4):418-22.
Campbell IA, Ormerod LP, Friend JAR, Jenkins PA, Prescott RJ. Six months versus nine months chemotherapy for tuberculosis of lymph nodes: final results. Respir Med. 1993;87(8):621-3.
Zada B, Durrani SN, Billah M, Iqbal J, Khan A, Nadeem M. Evaluation of Treatment Efficacy of Surgical Interventions for Tubercular Cervical Lymphadenopathy. Pak J Med Health Sci. 2022;16(10):752-52.
Kimura Y, Shimada M, Kawashima M, Yamane A, Nagai H, Matsui H. Relapse of cervical tuberculous lymphadenitis immediately after completion of effective anti-tuberculosis treatments. Respirology Case Rep. 2020;8(4):00555.
Tahiri I, Yacoubi R, Elhouari O, Anajar S, Loubna T, Hajjij A, Zalagh M, Snoussi K,
Essaadi M, Benariba F, Ilias T. The Role of Surgery in the Treatment of Cervical Lymph Node Tuberculosis. Cureus. 2023;15(5).
Kamal MS, Hoque MHE, Chowdhury FR, Farzana R. Cervical tuberculous lymphadenitis: clinico-demographic profiles of patients in a secondary level hospital of Bangladesh. Pak J Med Sci. 2016;32(3):608.
Jha BC, Dass A, Nagarkar NM, Gupta R, Singhal S. Cervical tuberculous lymphadenopathy: changing clinical pattern and concepts in management. Postgrad Med J. 2001;77(905):185-7.
Hegde S, Rithesh KB, Baroudi K, Umar D. Tuberculous lymphadenitis: early diagnosis and intervention. J Int Oral Health. 2014;6(6):96.
Atnafu A, Wassie L, Tilahun M, Girma S, Zenebe Y, Beyene MA, Alemu A, Fisseha E, Agze H, Desta T, Desta K. Microbiological Investigations of Fine Needle Aspirates from Newly Suspected and Previously Treated Tubercular Lymphadenitis Patients. Infect Drug Resist. 2023;3453-3461.
Ghariani A, Jaouadi T, Smaoui S, Mehiri E, Marouane C, Kammoun S, Essalah L, Driss M, Messadi F, Slim-Saidi L. Diagnosis of lymph node tuberculosis using the GeneXpert MTB/RIF in Tunisia. Int J Mycobacteriol. 2015;4(4):270-5.
Kanjanopas K, Siripan N, Phoophitphong R. Tuberculous cervical lymphadenopathy and the role of surgical treatment. Southeast Asian J Trop Med Public Health. 2014;45(6):1419.
Omura S, Nakaya M, Mori A, Oka M, Ito A, Kida W, Inayoshi Y, Inoue A, Fuchigami T, Takamori M. A clinical review of 38 cases of cervical tuberculous lymphadenitis in Japan–the role of neck dissection. Auris Nasus Larynx. 2016;43(6):672-6.