Assessment of psychiatric co-morbidities in patient of interstitial lung disease attending a tertiary medical centre
Assessment of psychiatric co-morbidities in patient of interstitial lung disease attending a tertiary medical centre
Abstract
Aims and Objectives: Interstitial lung disease (ILD) is a diverse group of conditions that are characterized by inflammation and fibrosis of the pulmonary parenchyma. In general, ILD is chronic and progressive diseases that result in substantial morbidity and mortality. The cardinal symptom of ILD is dyspnea; however, other pulmonary and extra-pulmonary symptoms are often present [1]. ILD is a common respiratory illness, in which some of the disease-related factors may increase the vulnerability to psychiatric disorders. This study was done to determine the prevalence of psychiatric co-morbidity in patients of ILD.
Methodology: It is an observational study conducted in 110 follow-up patients of Interstitial lung disease attending respiratory medicine OPD at a tertiary care center in central India. Psychiatric comorbidities are assessed by a pre-designed short structured questionnaire using Mini international neuropsychiatric interview.
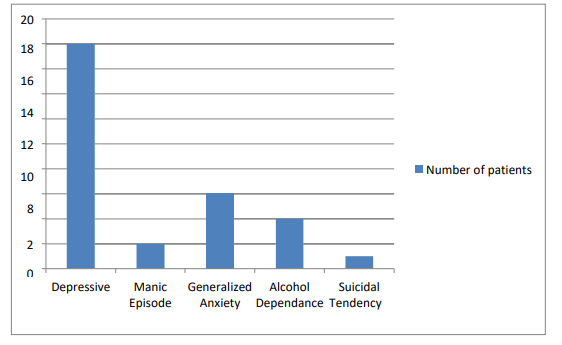
Result: Among 110 patients of ILD 28% had psychiatric co-morbidity mainly depressive episodes (59%). A significant association is found between upper socioeconomic status (P =0.01), duration of active illness (more than 1 year) (P =0.001), and age of patient between 40 to 60 years (P =0.001) with psychiatric co-morbidity of ILD patient.
Conclusion: Our study shows there is an increased prevalence of psychiatric co-morbidities in patients of ILD, higher than the national average. The predominant psychiatric disorder seen is depressive disorder, so treatment of ILD should be a multidisciplinary approach including medical treatment of ILD and psychiatric evaluation to prevent psychiatric comorbidity or its early management. This will greatly reduce the morbidity, visits to hospitals, expenditure on treatment and thereby having better outcomes in our patients of ILD.
Downloads
References
American Thoracic Society/European Respiratory Society American Thoracic Society/ European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonia, Am. J. Respir. Crit. Care Med. 165 (2002) 277–304.
Lederer DJ, Martinez FJ. Idiopathic pulmonary disease. N Engl Med.2018; 378:1811–1823.
Hutchinson J, Fogarty A, Hubbard R, et al. Global incidence and mortality of idiopathic pulmonary fibrosis: a systematic review. Eur Respir J. 2015; 46:795–806.
Holland AE, Hill CJ, Glaspole I, et al. Predictors of benefit following pulmonary rehabilitation for interstitial lung disease. Respir Med.2012;106(3):429–435.
K.A. Riekert, S.J. Bartlett, M.P. Boyle, et al, The association between depression, lung function, and health-related quality of life among adults with cystic fibrosis, Chest 132 (2007) 231–237.
W. Katon, M.Y. Fan, J. Unutzer, et al, Depression and diabetes: a potentially lethal combination, J. Gen. Intern.Med. 23 (2008) 1571–1575.
Lee YJ, Choi SM, Lee YJ, et al. Clinical impact of depression and anxiety in patients with idiopathic pulmonary fibrosis. PLoS One.2017;12(9):e0184300.
Ryerson CJ, Berkeley J, Carrieri-Kohlman VL, et al. Depression and functional status are strongly associated with dyspnea in interstitial lung disease. Chest. 2011;139(3):609–616.
Holland AE, Fiore JF Jr, Bell EC, et al. Dyspnoea and comorbidity contribute to anxiety and depression in interstitial lung disease. Respirology. 2014;19(8):1215–1221.
Ryerson CJ, Arean PA, Berkeley J, et al. Depression is a common and chronic comorbidity in patients with interstitial lung disease. Respirology. 2012;17(3):525–532.
Coelho AC, Knorst MM, Gazzana MB, et al. Predictors of physical and mental health-related quality of life in patients with interstitial lung disease: a multifactorial analysis. J Bras Pneumol. 2010;36(5):562–570.
Akhtar AA, Ali MA, Smith RP. Depression in patients with idiopathic pulmonary fibrosis. Chron Respir Dis. 2013;10(3):127–133.
Glaspole IN, Watson AL, Allan H, et al. Determinants and outcomes of prolonged anxiety and depression in idiopathic pulmonary fibrosis. Eur Respir J. 2017;50(2): pii: 1700168.
M.E. Kunik, K. Roundy, C. Veazey, et al, Surprisingly high prevalence of anxiety and depression in chronic breathing disorders, Chest 127 (2005) 1205–1211.
S.F. Taghreed, R.H. Manal, E. Taghreed, I.A. Omaima, Anxiety, and depression among patients with Bronchial asthma, chronic obstructive pulmonary disease, and diffuse parenchymatous lung diseases, Egypt. J. Hosp. Med. 49 (2012) 718–731.
B. Lo¨ we, K. Gra¨ fe, C. Ufer, et al, Anxiety and depression in patients with pulmonary hypertension, Psychosom. Med. 66 (6) (2004) 831–836.
K.O. Lindell, E. Olshansky, M.K. Song, T.G. Zullo, K.F. Gibson, N. Kaminski, L.A. Hoffman, Impact of a disease management program on symptom burden and health-related quality of life in patients with idiopathic pulmonary fibrosis and their care partners, Heart Lung 39 (4) (2009) 304–313.