Clinical utility of Continuous Positive Airway Pressure (CPAP) in Respiratory Distress Syndrome (RDS) babies and their complications.
Abstract
Background: Respiratory distress syndrome (RDS) historically called hyaline membrane disease is mainly a developmental disorder of preterm neonates due to structural immaturity of the lungs and surfactant deficiency. The incidence of RDS is inversely proportional to gestational age and birth weight. Despite recent advancements, RDS is still the most common cause of morbidity and mortality in the newborn group.
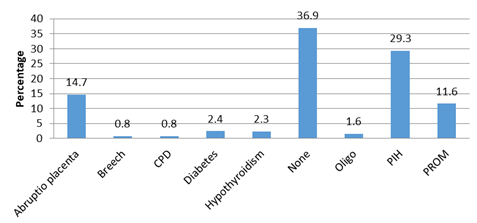
Methods: It was a descriptive longitudinal observational study including all preterm neonates with 30-37 weeks’ gestational age and grade 1 & 2 RDS and was conducted over 2 years’ duration at a tertiary level setup.
Results: 97 neonates managed only with CPAP, all had good outcome. Out of 19 neonates managed by CPAP+ surfactant,18(94.7%) had good outcome. Out of 6 neonates managed by CPAP+ Surfactant+ Mechanical ventilation, 2(33.3%) had a good outcome and 8 neonates were managed by CPAP+MV of which 4(50%) had good outcome. 43.8%(57) preterm RDS neonates were given early CPAP and 56.2% (73) were given late CPAP. The success rate in case of early CPAP was 54 (94.7%), whereas in case of late CPAP, it was only 62(84.9%) out of 73. In early CPAP, 3 patients (5.3%) required surfactant and ventilation whereas in late CPAP 22 patients (30.1%) required surfactant and 11 (15.1%) required ventilation. Overall mortality in early CPAP was 3.5% whereas in late CPAP it was 9.6%. Only 1.7%(2) developed pneumothorax in CPAP success and 28.6%(4) developed pneumothorax among CPAP Failure cases.
Conclusion: Antenatal steroids not only play a role in reducing the severity of RDS but also in their good outcome. Early CPAP in comparison to late CPAP has a maximum survival rate, minimum mortality rate, less requirement of surfactant and ventilation support and CPAP success rate was high. Nasal trauma due to CPAP was directly related to the duration of CPAP application.
Downloads
References
Meherban Singh. “Care of the Newborn”. eight editions. chapter 19. Respiratory disorder. pg no 359.
Lemons JA, Bauer CR, Ohw et al. Very low birth weight babies outcome of the National Institute of Child Health and human development neonatal research network. Pediatrics, 1996; 107(1): e1.
Whitsett JA, Pryhuber, GS ,Rice WR, Warner BB, Wert SE. Acute Respiratory Disorders. In: Avery GB, Fletcher MA, Mac Donald MG(eds), Neonatology: Pathophysiology &management of newborn 4ed philedelphia JB lippincott company;1994 :429-452.
Report of the National Neonatal Perinatal Database. National Neonatology Forum, India; 2002-03.
Fanaroff AA et al “Trends in neonatal morbidity and mortality for very low birth weight infants.” Am J Obstet and Gynecol 196;147d;2007.
Papadopolous MD, Swyes PR. Assisted ventilation in terminal hyaline membrane disease. Arch dis child 1964;39:481-484.
Cooke R, Lunding M, Lambolt RG et al. Respiratory failure in newborn. The technique & results of Intermittent Positive Pressure Ventilation. Acta Ped Scand 1967;56:498-508.
Adamson TM, Collins LM, Dehan M et al. Mechanical ventilation in newborn infants with respiratory failure. Lancet 1968; 2: 227- 31.
Gregory GA, Kitterman JA, Phibbs RH et al. Treatment of idiopathic respiratory distress syndrome with continuous positive airway pressure. N Engl J Med 1971;284:1333-40.