Study of growth outcome in Neonate born by eclampsia and pre-eclampsia in a rural tertiary care hospital in western Maharashtra
Abstract
Aims and objectives: To study the growth outcome of neonates born by eclampsia and pre-eclampsia mothers in rural tertiary care hospital.
Materials and methods: This was a hospital based descriptive type of cross-sectional study in Dr. Vitthal Rao Vikhe Patil Pravara Rural
Hospital, Loni. It was carried out over a period of 1 year that is from September 2022 to September 2023.All neonates born to pre-eclampsia
and eclampsia mothers being admitted in Dr. B V P Pravara Rural Hospital were included in the study.
Babies born with Congenital malformation and those born to mothers with other problems like rhesus incompatibility, severe anemia, renal
disease, heart disease, connective tissue disease were excluded from the study.
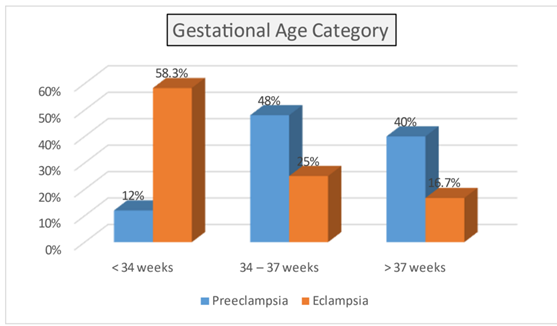
Results: Three fourth of the pregnancy induced hypertension mothers in our study were preeclampsia while one fourth were eclampsia. In the present study 65% babies were preterm , 34% babies were more than 37 weeks, 54.5% babies were born via normal vaginal delivery 45.5% babies were born via caesarean section, 6 %were <1kg birth weight ,14% were in 1-1.5 kg range,79 % were in >1.5 to 2.5 kg range. In preeclampsia group 18.65% were in IUGR group whereas 81.35% are not in IUGR group. In Eclampsia group 54.15% were in IUGR group whereas 45.85% are not in IUGR group.
Conclusion: Babies delivered to hypertensive mothers are more likely to experience a variety of difficulties, it is important to closely monitor these infants in an effort to reduce morbidity and promote better growth, development, and survival.
Downloads
References
Gruslin A, Lemyre B. Pre-eclampsia: fatal assessment and neonatal outcome. Best pract Res Clin Gynaecol. 2011;25(4):491-507.
Hypertension in pregnancy. Report of the American College of Obstetricians and Gemmologists Task Force on Hypertension in Pregnancy. ObstetGynecol. 2013;122(5):1122-31.
Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A.Maternal morbidity associated with early-onset and late-onset preeclampsia. Obstet Gynecol. 2014;771-81.
Berhe AK, Ilesanmi AO. Effect of pregnancy induced hypertension on adverse perinatal outcomes in Tigray regional state, Ethiopia: a prospective cohort study. BMC Pregnancy Childbirth. 2020;20(7).
Yilgwan CS, Pam VC, Yilgwan G. Comparing neonatal outcomes in women with preeclampsia and those with normal pregnancy. Niger J Paediatr. 2020;47(3):258-63.
Lawrence ER, Beyuo T, Kobernik E K. A comparative analysis of neonatal outcomes inpregnancies complicated by preeclampsia andeclampsia in Ghana. Am J Obstet Gynecol Glob Rep.2022;2.
Stefanska K A, Zielinski M, Joanna. Perinatal and neonatal outcome in patients with Preeclampsia.Ginekologia Polska. 2022;93(2):203-8.
McKenzie KA, Trotman H. A Retrospective Study of Neonatal Outcome in Preeclampsia at the University Hospital of the West Indies: A Resource limited Setting. J Trop Paediatrics. 2019;65:78-83.
Ramya C, Kumari R, Chitneni C. An observational study of early neonatal outcome in babies born to mothers with pregnancy induced hypertension. Int J Contemp Pediatr. 2020;7(8):1781-6.
Bossung V, Fortmann MI, Fusch C, Rausch T,Herting E, Swoboda I, Rody A, Härtel C, Göpel W,Humberg A. Neonatal Outcome After Preeclampsia and HELLP Syndrome: A Population-Based Cohort Study in Germany. Front Pediatr. 2020;8:579293.
Atamamen TF. Systematic literature review on the neonatal outcome of preeclampsia. Pan Afr Med J. 2022;41(82).
Moawad EMI, Tamm ASF, Mosaad MM, Sayed HME, Atef A. Evaluating the predictive value of fetal Doppler indices and neonatal outcome in late onset preeclampsia with severe features: a cross sectional study in a resource limited setting. BMC Pregnancy and Childbirth. 2022;22:377.
Tousty P, Fraszczyk-Tousty M, Ksel J. Adverse Neonatal Outcome of Pregnancies Complicated by Preeclampsia. Biomedicines. 2022;10:2048.
Powe CE, Levine RJ, Karumanchi SA. Preeclampsia, a disease of the maternal endothelium:the role of antiangiogenic factors and implications for later cardiovascular disease. Circulation. 2011;123(24):2856-69.
Mutter WP, Karumanchi SA. Molecular mechanismsof preeclampsia. Microvasc Res. 2008;75:1-8.
Knuist M, Bonsel GJ, Zondervan HA. Intensification of fetal and maternal surveillance in pregnant women with hypertensive disorders. J Gynecol Obstet. 1998;61(2):127-33.
Burrows RF, Andrew M. Neonatal thrombocytopenia in the hypertensive disorders of pregnancy. Obstet Gynecol. 1990;76(2):234-8.
Mouzinho A, Rosenfeld CR, Sanchez PJ. Effect ofmaternal hypertension on neonatal neutropenia and risk of nosocomial infection. Pediatrics.1992;90:430-5.
Wu CS, Nohr EA, Bech BH. Vestergaard. Health of children born to mothers who had preeclampsia: a population-based cohort study. Am J Obstet Gynecol. 2009;201(3):269.
Backes CH, Markham K, Moorehead P, Cordero L, Nankervis CA, Giannone PJ. Maternal preeclampsia and neonatal outcomes. J Pregnancy. 2011;214365